In the spirit of public Q&A, I’m sharing an intriguing question I received recently from a community colleague. Check out my answer and then add your ideas and suggestions in the comments below. Do you know of any particularly good or interesting services to empower patients in their relationships with doctors, especially ones which involve […]
Smart Patients
How did you find your people?
The internet gives us access not only to information, but also to each other. That deceptively simple insight, gained from years of research, contains so much of the hope I have for the future of health and health care. When we get sick or receive a new diagnosis, we often feel alone, but we shouldn’t. […]
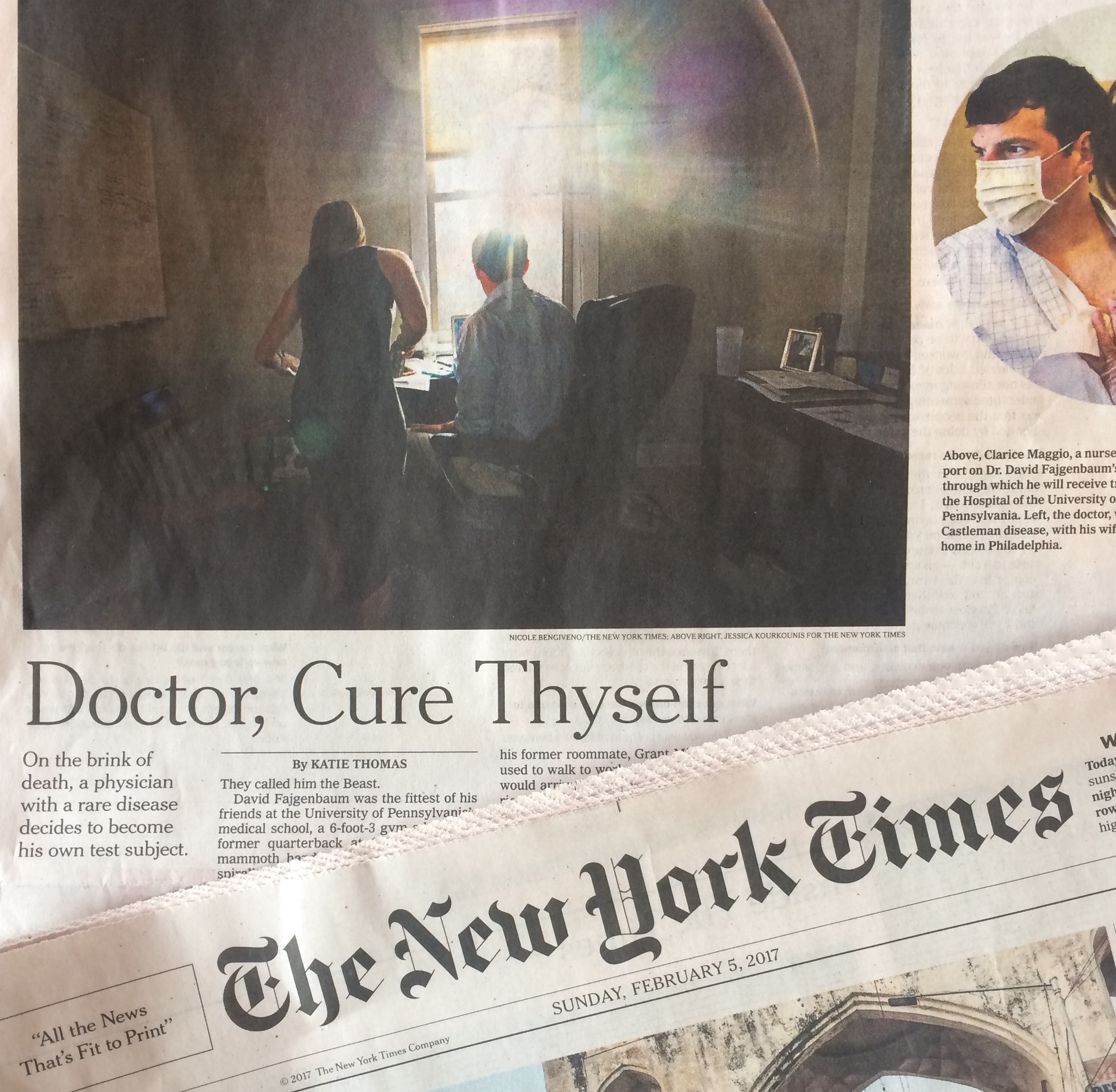
“His doctors were stumped. Then he took over.”
How might we empower people to participate in research about their own diseases or conditions? Which models work best for organizations solving medical mysteries or improving care for those living with rare conditions? These are two of the questions raised by a New York Times story today: “His doctors were stumped. Then he took over,” by Katie Thomas […]
Parkinson’s For One Day
My new job is wonderfully immersive. I leave home early, come back late, and, in between, spend hours talking with people about the future of health, health care, and technology (broadly defined). The HHS IDEA Lab blog will be my outlet for sharing ideas related to the work I do there. This site will serve, as it […]
What I’ve been working on
It’s been a busy few weeks and I’d love to share a few items in one post: I served as the emcee at the Robert Wood Johnson Foundation‘s Data for Health report release event. I attempted to capture the spirit of the event in this Storify. Here’s a post I wrote about the Data for Health initiative: Imagining […]
Cystic Fibrosis For One Day
I shadowed a mom and her 5-year-old with CF from afar for 24 hours. It taught me more than I could have imagined about living with a life-shortening disease — and about myself. This “empathy exercise” was organized by Smart Patients, an online community where patients and caregivers learn from each other.



Recent Comments