I’m honoring the contributions of my community colleagues over the years by pulling out some of their best comments and quotes. Jack Penner, in response to “His doctors were stumped. Then he took over” (2017): In terms of how can we empower patient to become active participants, one thing that comes to mind is lowering […]
net-friendly docs
What do you keep nearby, to inspire you?
Tom Ferguson, MD, gave me this robot in 2002, part of the first (and only?) fourth class of awardees of the Ferguson Report Distinguished Achievement Awards. I have kept it on or near my desk ever since. Reading Tom’s old essays, even as far back as the 1970s, is humbling. He foresaw so much of the world […]
A thank you note to Jordan Grumet, MD
Dear Jordan, You begin your book with a beautiful description of your public writing as a love letter to your patients and to your father, who died suddenly when you were seven years old. My heart opened at that moment and I saw you in a new light. I’ve read your blog and followed your story […]
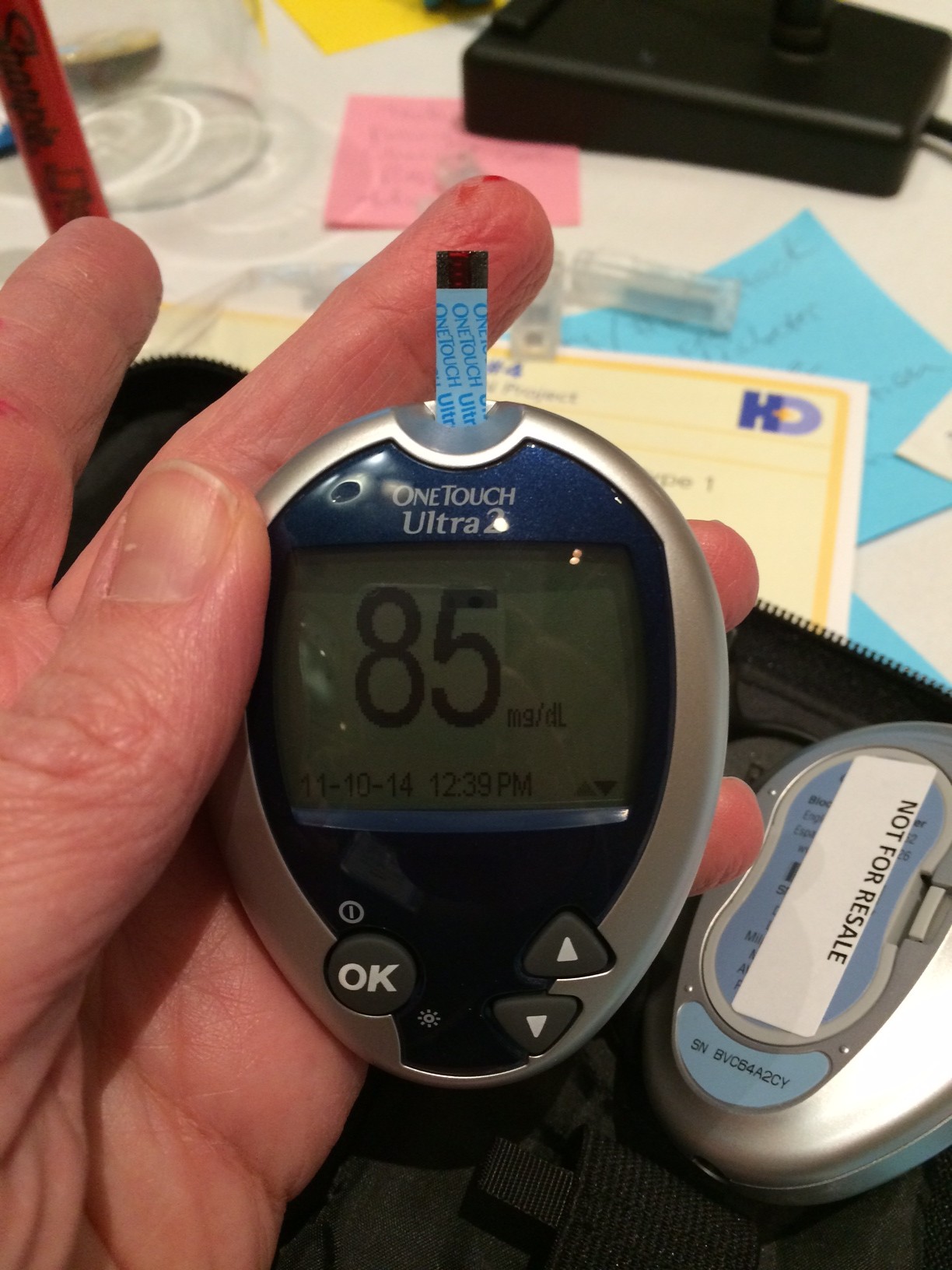
Imagining better outcomes for T1D with #MakeHealth
This post originally appeared on Diabetes Mine. Forty-five makers, thinkers, designers and doers gathered in Cincinnati for a two-day meeting to kick off “Phase Zero” of a new initiative to imagine a new system of care for people living with Type 1 diabetes (T1D). The best way I can describe the group is that everyone […]
“We just flipped a switch.”
“At one level, we just flipped a switch. It wasn’t a complicated, multi-faceted, variegated intervention. All we did was open up the doctor’s notes… Out of that came a cascade.” – Tom Delbanco talking about OpenNotes and how a seemingly simple change — allowing patients to view clinicians’ notes from their visits — is having […]
Put down the clipboard and listen
Here are the remarks I prepared for the Feb. 6, 2014, Engage & Empower Me class at Stanford Medical School. It’s a long post, so if you’d prefer to zone out, you can watch the video. In thinking about this class, I thought a good framing question for tonight is: How does change happen? How […]


Recent Comments