Amy Gleason (@ThePatientsSide) captured this line of mine, delivered on a panel at the Health Datapalooza yesterday. Her tweet generated an interesting cascade of reactions ranging from: “This is potentially dangerous” to “This is obvious (and old news).” I thought I’d expand on my observations and see if people want to expand on theirs in the comments.
First, this IS an old idea and not original to me. It was planted in my head by Tom Ferguson, MD, in 2001 and then nurtured throughout the early 2000s by pioneers like Danny Sands, Terry & Joe Graedon, Dan Hoch, John Lester, Alan & Cheryl Greene, Gilles Frydman, John Grohol and others back in the day. Famously, Danny gave E-patient Dave an actual piece of paper with “ACOR.org” written on it in 2007.
Second, I attend conferences is to be introduced to new ideas and to test the validity of old ones by saying them out loud in a crowded room. I only wish our panel had been recorded so we could capture all the great insights that were shared by David Fajgenbaum, Bon Ku, and our colleagues in the audience.
Third, in case anyone had any doubts: People seeking, finding, and creating peer health advice online is an unstoppable trend that I’ve been tracking for (yikes) 20 years. Here’s my research page if you’d like to dig in.
Fourth, a huge cottage industry of peer-to-peer health communities has sprung up whether anyone likes it or not. There are Facebook Groups, Reddit threads, and Twitter hashtags. There are glossy, corporate-backed platforms. There are old-school forums and list-serves. Some peer communities pop up for an event or acute situation, others sustain over many years. All of them ladle out support, many engage in discovery and problem-solving, some are saving lives. And there is a growing body of literature mapping and measuring the impact of peer-to-peer health.
But peer health advice and connection still hasn’t tipped over into the mainstream, which I think will happen when clinicians recommend it to their patients (Paul Wicks warns that “one day, it’ll be malpractice for a newly diagnosed patient not to be connected to 5-10 other patients like them in the first 12 months.”)
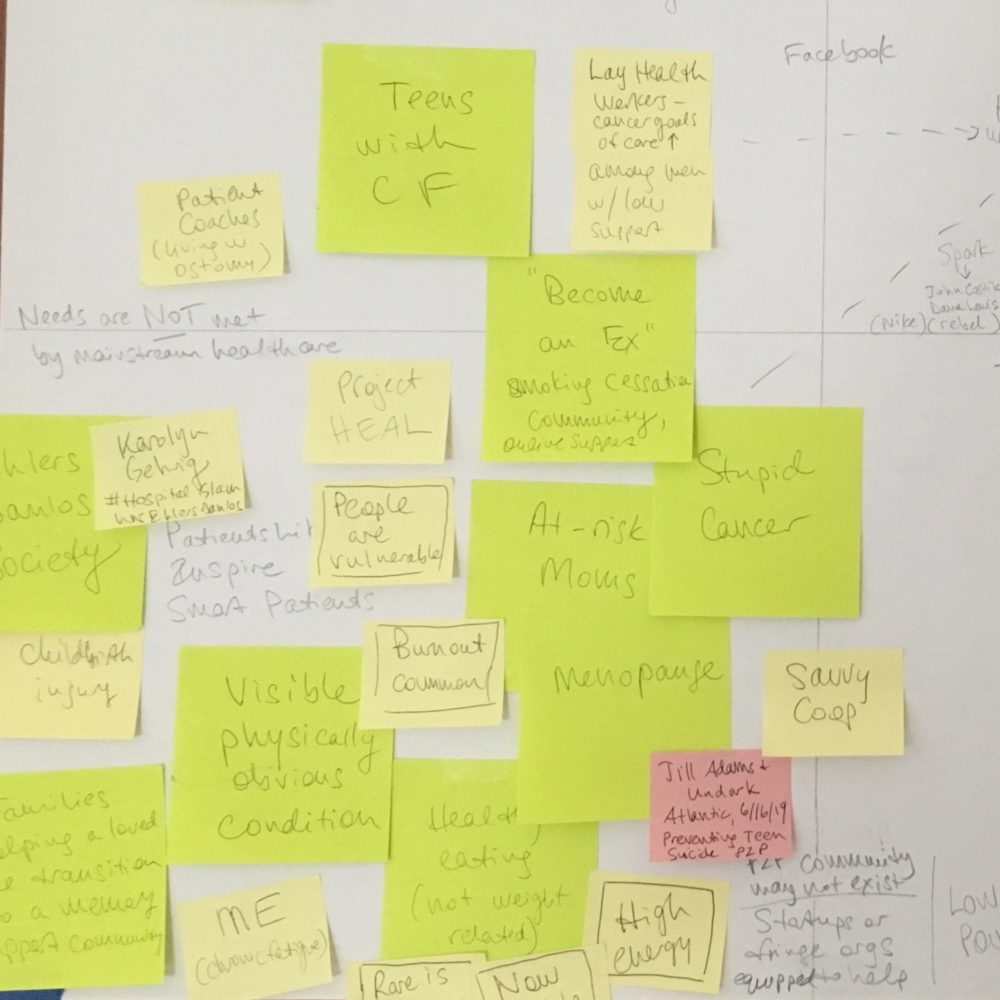
I’m working on a model to try to explain this phenomenon to people just tuning in and my office walls are covered with my hand-drawn diagrams of dyads and examples. We suffer from a glut of great stories but no map.
In the spirit of crowd-sourcing questions, not answers, I’d like to share a few of the ways I am stretching out the tangle. Where along these spectrums does YOUR favorite peer health community fall? What dyads do you suggest adding?
Acute, fast-moving, even emergency situation <—-> Chronic, even life-long condition
Temporary community <—-> Long-term community
People’s questions are NOT being answered by mainstream health care <—-> People are well-served by mainstream institutions
Data about the condition is excellent and available to share <—-> Data is non-existent, incomplete, not shareable
Treatments are well-known to be safe and effective <—-> Treatments are seen to be risky
Home care is at the center of the patient experience <—-> Care delivery happens in a clinical setting
Solutions are low-tech <—-> Solutions require advanced tech
Now: your turn. Comments are open.
Note: I try to remember to use the inclusive term “clinicians” so I updated the title of the post to reflect that, instead of the original “doctors.”
Featured image: The most crowded and fruitful quadrant of all the 2×2 diagrams in my office.
I don’t know how this thought fits into your scheme…what comes first to mind for me, as the fortunate one with only minor medical issues at age 67…is the notion of decision trees. Since I don’t know what I don’t know, and I have a ringside seat to a spouse with significant health issues that over the years have proven extremely difficult to diagnose and address, the dyad of narrow to broad comes to mind. Is the resource a rabbit hole, or is the resource broad enough in membership or milieu so that queries range wide?
Thank you! I love that perspective!
I hope this comment gets to you Susannah. I’m not so tech savvy. I am the wife of a PD husband. His DX was 11 years ago. Besides the incredible amount of info in Smart Patients for caregivers and PD patients which I believe is very valuable despite what some say about misinformation there is another very invaluable aspect. That is knowing we are not alone and I feel I am getting the support which helps me maintain my sanity. I am bipolar and have other chronic diseases. There is no one on earth who can have the empathy like someone who is walking in my shoes. I believe that is critical support for anyone experiencing any hardship.
Thank you, Alex, it did get to me! Sorry for the delay in approving it (an anti-spam feature means I need to approve all first-time commenters or any comment with links). I so appreciate your sharing your experience!
At a recent talk I gave at an NGO meeting regarding cancer healthcare hashtag communities two oncologists after the talk told me they plan on sharing the cancer communities on Twitter with their patients. It is slowly happening.
Here are some dyads to add to your list.
We know things that can reduce our risk for X –> We don’t know enough about how to reduce risk for X
This website/ group has links to peer reviewed journals –> this website/ group just shares information no link to sources
this community includes patients and health care professionals —> this community includes patients only
Dee, thank you. I wonder if specialists are more likely than generalists to see the possibility of crowdsourcing and peer support. If I had the budget I’d survey various groups of clinicians — nurses, physical therapists, pediatricians, radiologists, oncologists, allergists…etc — and ask if they have recommended online resources (including peer communities) to patients.
And I love those dyads!
Susannah,
I love this post! I love the systematic, patient, evident-based responses 🙂
I wanted to share a few resources in case you were not aware of them. In my non-profit work this past year, especially related to equipping trusted messengers for the 2020 Census, we have been looking for/at asset maps and network maps. Here is an example (https://recovertogether.withgoogle.com/) from Google related to mental health (and the related article: https://www.worth.com/how-data-can-help-cities-tackle-addiction-and-mental-health-crises/). You might also find the practice of appreciate community building applicable (see excerpt from: https://aipractitioner.com/2017/12/11/appreciative-community-building/):
“As BakerRipley approached its 100th year, we began to question the “needs-based” model. The issue became particularly clear as we started working in Gulfton – a richly diverse neighbourhood in southwest Houston full of hopeful, ambitious immigrants that represented the kind of community we could increasingly expect in the future. Focusing on what was “needed” or “broken” seemed inadequate when facing people so full of promise.
We knew the people we serve possess strengths and talents that went undiscovered when we only assessed what they needed. We saw people with amazing inner resources and abilities, and recognised they were seeking opportunities to fulfill their aspirations.
We shifted our focus to the powerful untapped strengths of people and communities – their assets. We searched for a system of identifying those assets and integrating them into our daily work. By doing so, we could assist people in choosing their own direction, finding their own solutions and building their own communities.”
Finally, you might find something useful on June Holley’s site, scroll down to Mapping (https://networkweaver.com/store/).
Thank you! I so appreciate this deepening of the conversation, Mary. Will dig into those links.
Formal communities focused on specific and deep topics of interest (e.g. patients like me) <---> emergent communities that arise out of other activities that spark natural affinities around similar circumstances & a broader set of shared needs (e.g. teens playing Fortnite playing together & also connect + share about depression, anxiety)
My previous comment was supposed to be a dyad between formal vs emergent communities (but some characters dropped out) —FYI.
Thanks, Pete! I think I fixed it — if not let me know. SUCH a good dyad to call out here.
I think this is a great idea. Probably would be easiest for subspecialist who are familiar with a single community they trust, like a rare disease or specific type of cancer. I wonder if some of the app prescribing apps like Xealth, RXhealth or even Allscripts would be able to add that to their workflow.
I like this way of thinking about patient communities. Most groups will fall on the spectrum between the two extremes. A few more thoughts:
Condition is rare, most clinicians are unaware/uninformed about it <--> condition is common, most clinicians follow a standard of care
Condition is stigmatized, patients don’t talk about it in public <--> patients with condition are supported by family, friends, public
Condition is generally unknown to public <--> condition has extensive public awareness and active, visible advocates/advocacy organizations
Sorry, the separators in my comments got lost when it published
Thanks, Janet! I fixed it — great points.
Thank you Susannah, love crowdsourcing questions. The dyad spectrums are really helpful.
Where’s the intersection of peer-to-peer health with care partner support systems? Consider a diagnosis of dementia. Persons living with dementia have formed peer-to-peer health communities as advocates. And there are lots of caregiver support groups. But what does peer-to-peer health look like WITH persons living dementia?
The growth of Memory Cafes here in Pennsylvania is an example: https://www.memorycafedirectory.com/memory-cafes-in-pennsylvania/ – happening in context of growth of Dementia Friends https://www.dementiafriendspa.org/ and Dementia-Friendly Community movement. https://www.swppa.org/dfgp/
But how can physicians and care teams tangibly support individuals living with dementia and their families in their community, promoting peer-to-peer health (on and off-line) and wellbeing?
Mapping dementia across the dyad spectrums you shared will be a great exercise. The one that stands out is the “treatments are well-known to be safe & effective vs. risky.” Setting aside Rx solutions to treating dementia syndrome, the challenge all along has been there is no treatment that a physician can really prescribe. (So they tend to under-assess cognitive function and under-diagnosis dementia until progressed).
And yet, there are certain things that can be done to invest in a system of supports for individuals and families earlier – and doing that together may be real source of power resides.
Along those lines, and related to Mary’s resources on appreciative community-building (thank you Mary!), I think of Cormac Russell on Asset-Based Community Development: https://www.nurturedevelopment.org/blog/abcd-approach/part-4-dont-health-problem-village-problem/
His critique is of “social prescribing” deserves more high-level discussion in the US. Efforts to “combat” social isolation and loneliness must not be institutionalized such that they only further disempower individuals and communities.
#ABCD would seem to blend perfectly with peer-to-peer health, where there’s power in togetherness.
Joe, thank you! I can’t wait to explore these links & ideas in more depth.
Thanks also for bringing in your experience & expertise with a quite different challenge than what I’ve personally been thinking about so far with this lens. I hope we can work toward a way of seeing the world in a new way that applies broadly.
Echoing Joe (echoing Cormac) I am very leery of institutionalizing peer-to-peer. Do we really want to give clinicians even more authority, as gatekeepers / endorsers of peer groups? They have more than enough to do without having to spend time figuring out which groups are “good”. And even if they have the time, I’m not sure why one might think that clinicians would be a better judge of peer groups than others. As we know, managing our lives, our health and wellness in the context of real life, is about much more than medicine.
Even the most caring and thoughtful clinicians are often unaware of the complexities of real-world care if they themselves aren’t dealing with these conditions in their own lives. (Susannah — as you know from our work with T1D and CF communities a few years ago.)
It would definitely make our (individuals / patients / family carers) work easier if we knew which peer-to-peer groups were “good”, so the idea of someone who is deeply informed rating such groups is very appealing. But, let’s not assume that that someone is a clinician.
Is the community moderated by a health professional?
At Smart Patients, we’ve found that, if there is clinician in the community, other members are less likely to share their experiences as they wait for the clinician to speak up first.
On the other hand, some healthcare organizations won’t refer their patients UNLESS the community is moderated by a healthcare professional.
At SmartPatients.com and at ACOR.org, patients and family members correct one another and improve on answers politely and with accuracy. They refer each other to experts and reputable scientific sources, and they explain what these things mean. Professional information is not lacking in our groups; it is provided by non-professionals and made easy for newcomers.
Robin, thank you for sharing your deep expertise with creating and nurturing vibrant, useful peer health communities!
Kevin, you are calling out an ESSENTIAL tension that I think is generally invisible. Are there any measures or studies to document the observation that people clam up around clinicians?
I shall have a think about how we can measure that in our communities.
Anecdotally, when we do have a clinician join one of our communities, the reaction is always mixed but never mild.
I think it would be helpful to know the patient’s goal(s) and then the clinician can make recommendations for patient groups. Some people just want social support. Others want to know everything possible that they can do in terms of treatment choices and lifestyle choices to improve their health and daily functioning. Others just want to follow their doctor’s advice and that’s it. For me, this choice was probably linked to desperation. I didn’t receive any information about what I could do to maximize my health and I refused to just “wait” for the cascade of secondary conditions to appear. Dyad? Not willing to make lifestyle changes —Very willing to make lifestyle changes
Thank you for your panel with David Fajgenbaum & Bon Ku at Health Datapalooza!
Thanks, Susan! I love those additional dyads. Is this the way you’d express the first one?
Patient’s primary goal is to find social support <---> patient’s primary goal is to explore treatment choices.
I’m not sure there are any patients that join social groups solely to find treatment options. Most also ask questions about support issues, such as dealing with treatment side effects.
Thanks, Janet. Mine is too stark a representation of the dyad that Susan is describing. If you or others have a way to write it (or your own take on the point) please share.
Yes. What Janet said. I can’t imagine a support group that doesn’t provide both.
I think the mission of the community and how it matches a patient needs ( support / treatment / information) at that time in their experience is key to whether the group is successful.
We (#gyncsm) just ran a chat on Cancer Pre-hab and Rehab. We had patients learn about something that many didn’t even know was available. We had professionals ( Phys therapists & gyn oncs) share how rehab / prehab works in their settings and where to go for that support. We had patients question the professionals and offer ideas.
We have never heard feedback in 6+ years that people did not want to tweet because a professional was on the chat but then again our community is public so that might in and of itself cause some people to hesitate to post.
For our next community survey, a question about our health care moderators impact on participation might be informative. I’ll keep that in mind.
As a member of Smart Patients I can say that the women in the OC group are very knowledgeable about treatments, new research and ready to help with emotional issues too. And moderators like Robin help insure that the content is accurate. For those who are not comfortable with a public platform I have recommended SP.
Fabulous and important discussion! To me clinician interactions have three dimensions: a pace or cadence, a strength of connection, and a depth of information.
Whenever a patient group offers more frequent interaction, stronger connection, OR deeper information and education — it is poor practice to omit sharing these known patient groups. And poorer practice not to know them.
I have MS and it took me 3 or 4 years before i got my shit together and found a group to attend. The group has been the most informative part of my health care related to MS.
Stack Overflow is an excellent resource for computer programmers looking for answers to their questions. One of the key reasons it works so amazingly well at answering those questions, is that it’s a crowd sourced answer platform, which means…
Questions get asked multiple times in different ways and all those various forms of the same question get answered in slightly different ways that are sensitive to those unique versions of the same questions. This means that people looking for information can ask search their question in whatever way it occurs to them and often find an answer.
It makes it possible to search for something complicated and find relevant information. This is only possible when you have a community of people with experience in the category interacting, and it leverages all those people, those who only have a little knowledge/experience and those with a lot.
Great post and discussion. I’ll throw in two dyads to consider. Whether the two sides are addressed within one peer community or across distinct ones I think these are important dimensions:
* technical support (e.g. treatment options, side effects…) sense making / values support / validation in community (e.g. approaches to end of life that come from “who you are” not “what medicine can do”, approaches to supporting a child with an illness…)
* “of healthcare” (see selves / seen as part of “healthcare”) “of community” (see selves / seen as outside of healthcare, perhaps even in opposition to healthcare)
my symbols were stripped out it seems…
* technical support (e.g. treatment options, side effects…) VS sense making / values support / validation in community (e.g. approaches to end of life that come from “who you are” not “what medicine can do”, approaches to supporting a child with an illness…)
* “of healthcare” (see selves / seen as part of “healthcare”) VS “of community” (see selves / seen as outside of healthcare, perhaps even in opposition to healthcare)
Sorry about the issues with characters being stripped out of comments — and sorry for the delay in approving comments sometimes.
I’m so grateful to everyone who is making the jump from Twitter or a newsletter that mentioned the post (thanks 33mail & Politico!)
There have been many great insights shared on Twitter by people who haven’t (yet) joined us here, so I’m going to capture their words below (and again, the invitation is always open to expand on these thoughts):
Matthew Zachary wrote: “We tried this consistently for years when I ran
@stupidcancer, which – at the time – has the most visited website of AYA cancer resource on the web. 1M uniques/month in its prime. Doctors were not the “Yelp” for online support. Nurses and social workers were.”
Tatyana Kanzaveli wrote: “There might be potential liability issues: what if your patient follows an advice from a group member you recommend and gets worse …
list of patient support groups with a language that protects a provider is doable though”
Richard James wrote: “@NPCQIC is trying to integrate patient support group referrals, such as to local @MLH_CHD groups, into annual #chd checkups”
Aaron Neinstein wrote: “Yes! This is so important. I do this all the time w referring my pts to #t1d groups. They have so much knowledge to share and can provide a level and depth of support I cannot. Huge opportunity to scale medical care beyond 20 min office visit.”
Marco Flavio wrote: “Peers can be there when clinicians cannot. And they have a different, deep understanding. It’s an essential part of being a patient.”
Harlan Krumholz wrote: “Many patients report that they have learned the most from others on the same journey. We should be enhancing the opportunity to make connections. @teaminspire @patientslikeme and others. I would like to see all patients connected with others facing similar challenges.”
Paul Wicks wrote: “One day, it’ll be malpractice for a newly diagnosed patient not to be connected to 5-10 other patients like them in the first 12 months. There is a dose-effect curve of friendship, no side effects, it’s practically free, and the peers benefit too.”
John Mandrola wrote: “Great for some problems. It’s a challenge for #afib, where the treatment is extremely individualized. I tell patients all the time that their friend with AF is TOTALLY diff from you. Also, patient forums often biased toward content experts’ choices. AF ablation, for example.”
Krumholz replied: “But still likely possibly that there are clusters of people in every condition; people who are similar, even digital twins… and lots more who can learn from each others.”
Baby Boomer Writer shared: “And get support/ways of coping, from another patient who truly understands. Especially in regard to a nuisance symptom, it’s so helpful to know someone who also experienced it, and can tell you it eventually goes away!”
Inga Drossart wrote: “I suffered a rare complication from SA node ablations: SVC Syndrome. Luckily, in a pt forum I found two other pts with this complication. It was good chatting with them. Same for pacemaker RR issues: got ideas how to optimize RR from active pts and later could help others.”
Naomi Kaufman Price pointed me to a tweet by Raj Ratwani: “Do you need a prescription for an app? Interesting article by @landmaad, @DBatesSafety and others in @Nature_NPJ proposing a framework for prescribing apps for patients and key areas of focus for success. Love the focus on workflow & other system factors. http://go.nature.com/37r0vK1”
Dr. Riyaz Shah wrote: “Nothing wrong with guiding patients to resources containing sensible advice. In a world of trolls and charlatans it’s actually helpful. I do it often however groups not as organised in UK as US. Wouldn’t use words “prescribe” because it implies a form of professional coercion.”
Henry Wei wrote: “Peer groups can be powerful; I witnessed this when my father went through his terminal cancer journey. Intimacy, trust & physician collaboration > tech. Eg @nkf has long had a nice *phone* program, matching those with kidney disease with peer mentors: NKF PEERS
Grace Cordovano wrote: “Besides connecting patients to #peerhealth, the platform needs to champion ethical use of patient data, protect #DigitalDignity.”
Elin Silveous wrote a long thread: “Rather than clinicians “prescribing” these, why couldn’t wouldn’t they be automatically generated in an #EHR, #EMR upon diagnoses? Community-based online support groups have been around since national health organizations started. Online groups since at least 1993. My concern is the rise of pharmaceutical-based and pharm funded online peer groups/patient groups that may be used to push meds. They are different than unbiased mutual support groups led by peers for peers. I have observed a FB Group for Normal Pressure Hydrocephalus in which new members are encouraged to “get a shunt as soon as possible” w/disregard to anyone’s personal set of circumstances or benefits/risks/costs assessments. You know I have been a proponent of online mutual support groups since my inception of and fostering them in the early ’90’s. But what I am observing now is that many peer-to-peer groups have an agenda or bias. That concerns me. A lot. They seem less about helping people make informed, empowered decisions about factors that may influence health, well-being or quality/length of life & more about pushing product & reliance on the medical system (my observation).”
Jay Parkinson wrote: “Yeah what if your doctor’s platform she uses added these as prescribable resources…hmmm…what if??” <-- this tweet triggered a great conversation which is worth clicking through to read.
MsWZ wrote: “@mrjdz had that in his post op binder! I was a little surprised. Also a page of sites the surgeon found credible. It felt comforting. I did pause at first expecting pharma ads and the whole “fake” site crap. Nope! Legit old school message boards.”
Phew! I did not know that this one line in a panel presentation would elicit such a fantastic, potentially meaningful conversation. The magic of social platforms!
Here’s one line of the many above that caught my eye:
Wouldn’t use word “prescribe” because it implies a form of professional coercion – Dr. Riyaz Shah
In the U.S., clinicians hold a place of honor in people’s regard. The Pew Research Center found that 74% of U.S. adults say they have a mostly positive view of doctors and 57% say medical doctors care about patients’ best interests all or most of the time.
If a clinician believes, based on the evidence they have reviewed, that their patient would benefit from an intervention (a vaccine, a drug, an exercise routine, a meditation practice, a peer support group…) why NOT use their power to recommend it?
Here’s further context that came to my mind — a quote from a 2006 Pediatrics journal article:
“Health care providers have a positive influence on parents to vaccinate their children, including parents who believe that vaccinations are unsafe. Physicians, nurses, and other health care professionals should increase their efforts to build honest and respectful relationships with parents, especially when parents express concerns about vaccine safety or have misconceptions about the benefits and risks of vaccinations.”
(Citation: Smith, Philip & Kennedy, Allison & Wooten, Karen & Gust, Deborah & Pickering, Larry. (2006). Association Between Health Care Providers’ Influence on Parents Who Have Concerns About Vaccine Safety and Vaccination Coverage. Pediatrics. 118. e1287-92. 10.1542/peds.2006-0923. )
Again, if a clinician has reviewed the growing literature about peer health advice’s positive effects and/or has experience with past patients who benefited from a peer mentor or group then don’t they have an obligation to share the information? (As Paul Wicks wrote: in the future it will be malpractice to NOT do so.)
I’ve been unable to find a central registry for online communities. Right now it is quite hard to find the various communities for some diseases (especially rare diseases) which are often spread across different platforms. I’ve talked to some of the disease specific organizations, but they tend to only link to their own internally generated materials.
I’d appreciate any suggestions for solving these problems. Thanks.
Larry
Try Symplur Healthcare hashtags
https://www.symplur.com/healthcare-hashtags/
For healthcare communities on Twitter. Maybe someone else knows a listing of other types of communities.
I work at a health care organisation that has decided as a general way of doing things to map resources in the community, of all sorts, and train our clinical teams in doing social prescriptions (or recommending community groups, resources, connecting patients) we believe that the only way to provide real health care and improve our patients well being is by understanding their overall social needs, which now are highly linked to loneliness, and connecting them to other non clinical resources. We just started last year and we have had amazing clinical and well being results in our patients as well as in our clinical teams.
Camila, I love hearing that this is becoming a practice — let’s hope it spreads.
Friends, thank you again for the wonderful conversation so far. I’d like to add this article to the mix:
Indicators of retention in remote digital health studies: A cross-study evaluation of 100,000 participants, by Abhishek Pratap et al.
Key quote from the discussion section: “The largest impact on participant retention (>10 times) in the present sample was associated with clinician referral for participating in a remote study. This referral can be very light touch in nature, for example in the ElevateMS study, it consisted solely of clinicians handing patients a flyer with information about the study during a regular clinic visit. This finding is understandable, given recent research showing that the majority of Americans trust medical doctors.”
I see this as fuel for those who see the good in clinicians recommending a peer-to-peer health community. Do you agree?
One thought to add to this marvelous string would be to leverage some of the insights from Ben Thompson’s Stratechery blog, which calls out the core benefits of aggregation theory. The potential for a community platform to systematically enable patients/consumers to: feel supported/be known; share perspective on common experiences; crowd source collective insights on patient preferences — and to collectively inform what matters in patient-centered care decisions….has the power to truly bring the patient voice into care decisions, through the development of real-time decision support tools — informed by the patient communities (and not other stakeholders with other agendas, perhaps). This would offer important data cathment and help inform some of the emerging Patient Value frameworks at a time when Medicare is going broke and self-management is the future. You could leverage a community platform for a broader purpose — to inform patient-defined value — if the communities real-time were capturing/defining their wants and needs, specific to their distinct situation (social, disease, personal preferences). I love the work coming out of Penn/David Asch and the power of leveraging social incentives to get more traction out of any patient community…so that the choke hold in bringing patient perspectives into care decisions is not a set EHR roadmap or cost-constrained system priorities. The work coming out of Stanford’s Presence program — focused on the science of forging trust and engagement in care interactions — also helps informs a path on how to bring insights from a patient community into decision making and care planning alongside clinicians.
I love this suggestion. The Stratechery blog is an excellent resource. I’m excited to check out Stanford’s Presence program and the Penn/David Asch work.
Wow! Thanks for sharing these resources, Nancy.