My phone started blowing up with texts from friends and family members yesterday morning, alerting me to a New York Times magazine cover story by Amanda Hess, “My Son Has a Rare Syndrome. So I Turned to the Internet” (gift link). Hess writes beautifully about her experience being dropped into the medical maze and her […]
Rare Disease
Rare Disease in the U.S. 2025
Rare disease communities welcomed me as a researcher, inspired me to highlight their ingenuity in my book, Rebel Health, and now I am honored to share results from the first probability-based national survey to measure the rare disease population. I partnered with my former Pew Research colleague Kristen Purcell, now at SSRS, to write the […]
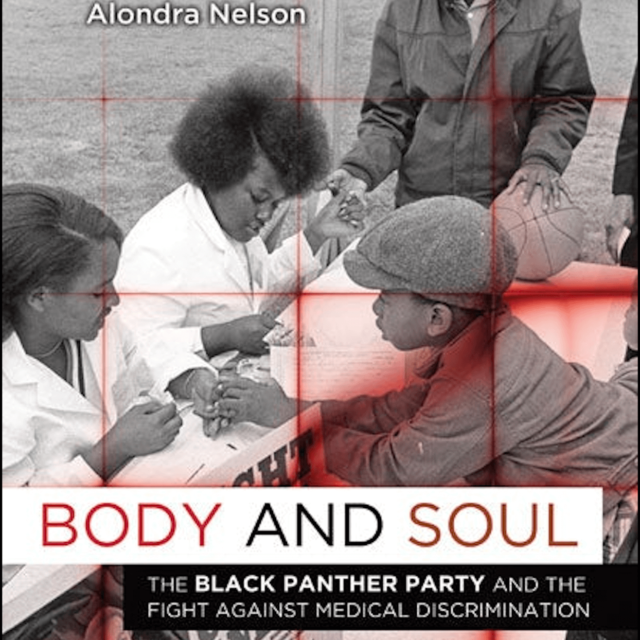
The Black Panther Party’s Health Innovations
Here is the 40th in my series of “Wow! How? Health” stories, also shared on LinkedIn if you want to follow the conversation on that platform. In 1971, the Black Panther Party diagnosed the federal government’s failure to study sickle cell anemia, a genetic disease believed at the time to be found predominately in people […]
Rebel Health on The Nocturnists
Today is the one-year anniversary of the publication of my book, Rebel Health. To celebrate, I am inviting you to listen to my favorite conversation about why I wrote it and what lessons we can all draw from the patient-led revolution. Emily Silverman, MD, is the host of The Nocturnists. She suggested that I start […]
Wow! How? Hope for Henry
Imagine being a little kid and facing not only serious illness, but all the uncomfortable, scary treatments associated with hospitalization: blood draws, IV placements, and scans. Then you find out that you can earn prizes for every medical procedure you go through, thanks to an incentive program called Super Rewards for Super Kids. Kids love […]
Public Q&A: Rare Disease and Rebel Health
The Global Genes RARE Advocacy Summit in September 2023 provided a forum for me to talk, for the first time, about my upcoming book and how rare disease communities have been a key part of my professional life. Here’s a set of questions that Sravanthi Meka of Global Genes asked me in advance of the meeting: […]





Recent Comments