I am a caregiver. I help coordinate the health and home care for an elder loved one who, for the purposes of maintaining a bit of anonymity, I will call “M.” He is a healthy, happy octogenarian. We have known each other for nearly 40 years, but we are not related by blood.
I am also an apprentice. My mother has been a primary caregiver for five people, each of whom presented very different challenges and yet all needed much the same care, particularly at the end. It has been an honor to assist Mom and learn from her about pattern recognition in elder and end of life care.
On Sunday morning I woke up early to start work (as a caregiver, I time shift a lot) but could not settle into my research until I captured what I call my Project Management Plan for M. I divided it into categories, each with proposed next steps, results, expected completion dates, etc.
Here are the categories (please ask questions and give me feedback in the comments below):
- Home care (for example, coordinating housekeeper visits)
- Community care (making sure his faith community is tuned in)
- Health care (finding someone who can take notes when M. visits his primary care doctor)
- Legal (making sure his advanced directive is up to date)
- Safety (discussing an emergency plan with M.)
- Joy (setting up flower delivery as a monthly luxury item)
But I know I could do a better job on my worksheet if I had more time, more peer input, more design skills.
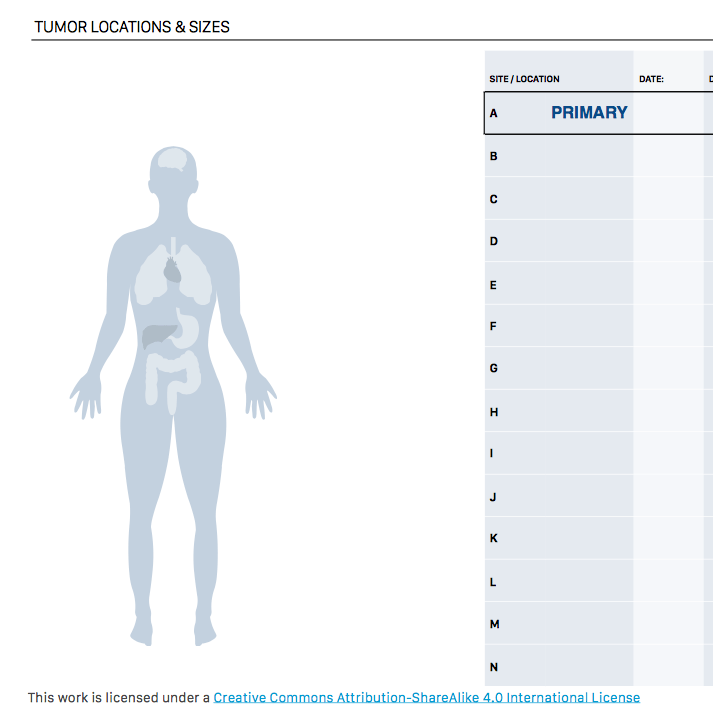
So when I took a break to look at Twitter, I was astonished to see a link to a Fast Company article about April Starr, a designer who created beautiful, useful worksheets for people being treated for cancer. She “solicited feedback from her widow grief group— peers who had been through similar battles with cancer—to see what they would like included” in a cancer worksheet.
This is exactly what I need, except for elder care. Does it exist? If not, let’s crowdsource the requirements that we would request.
For example, @MsWZ wrote in a tweet:
“Ex: stuffed fridge w expired products = early warning sign of things changing.
Means they need community, likely good to do a depression check, and meals and tips on shopping for 1-2 adults, not 5-6. Not newlywed cookbooks
Doesn’t mean they need a group home or a day nurse.”
What would you add? Please join me in the comments below.
Featured image: A detail of one of Starr’s worksheets. You can download the full set at: cancerworksheets.com
Someone to handle their meds management – getting them enrolled in a prescription delivery service (like Pill Pak), or just showing up once a week to sort their meds out and to see that they are their meds (set up text reminders or if really tech savvy, have Alexa remind them). Set up meal delivery services a few times a week with Meals on Wheels and volunteer drivers in your community for medical transport.
Terrific ideas! I confess I don’t even know if M. takes any medications, but now I’ll ask (we are still early in our carer/caree relationship).
Another one from David Goldsmith, who tweeted:
“Going to channel @healthythinker here and add “financial wellness” to your categories. Sharks prey on vulnerable and frail people all day long. Look at checks and credit card charges. Check EOBs, etc. Someone needs to keep very close tabs on this part of caregiving.”
(For those who don’t know her, Jane Sarasohn-Kahn is @healthythinker.)
Alexandra Drane makes a couple of great points in her tweet:
“And with one in four caregivers being millennial and 50% of them male, a great need to expand our definition of who to be keeping an eye out to help! Most important tool? #LOVE Be always on the look out to love on a #caregiver”
So true.
I’m a neuroendocrine cancer survivor myself (dx at 56) and was quite struck by the helpfulness and aesthetic niceness of these worksheets. The Los Angeles chapter of our principal cancer support organization did its own worksheet designing for exactly the same reasons but I think neither the designer nor the LA chapter knew about the other! I am definitely sharing a link to our FB group pronto. Thanks for sharing.
How wonderful! I’ll ping April to let her know. Thanks for stopping by to comment and best wishes for continued good health.
Some years ago I had come across “Caring for Mom: A Practical Resource for Caregivers”, full of worksheets and checklists that seemed well designed. It’s written by Diane Moore, and still available for free download here: https://caringformom.org
Wow! What a great resource book!
I should note that one of the first tasks I completed with M. was an Atlas CareMap (categorized as both Community and Health Care on my worksheet 🙂
The other exercise we did early on was to go through the 5 questions developed by Engage with Grace. M and I have both been bedside for the death of loved ones in the past few years so an end-of-life discussion was right at the surface and, although it may sound odd to some people, a great ice-breaker for us as we deepen our relationship. (Categorized as Health Care on my worksheet since the choices often intersect with the health care system.)
Thanks so much for starting the conversation!
I would add:
Preferences: Meals, clothes, schedule, medical care, socialization, restaurants, excursions. Helpful to know so anyone providing care can create what a caree needs and wants.
Comfort: Songs, prayers, books, movies, TV. This could be similar to joy but I think of it more as what brings comfort during difficult days and moments.
Success: What a caree does well, including use of technology, adaptive gadgets, activities, hobbies, interests. Again, could be similar to joy but helpful to know whether or not a caree uses an iPhone (my parents are 88 and 85 and love theirs), can make a great sandwich, can manage their own care with the help of certain devices. It’s so helpful when we can keep their successes in their day.
Beautiful, Denise. Thank you. (And may I say I am humbled by your coming to comment on this thread — your work is a constant source of inspiration to me.)
One more suggestion: One of my members posted a list she compiled in order to be reimbursed for caring for her mom which you may find helpful: https://www.caregiving.com/2017/05/caregiving-task-list/
Always so happy to spend time with you, Susannah! Thanks for inviting all of us to share and explore the possibilities.
That’s quite a list. Thank you!
On a lighter (?) note, it reminds me of the job posting for a “household manager/cook/nanny” that went viral in January. The detail of it (and intriguing focus on fish math) was easy to lampoon but I agree with some observers who said that it captured the invisible work that goes into running a household with children. There is so much invisible caregiving work! Who would have thought to list toe nail care? But wow is that important, as we who have clipped the nails know.
I would like to add not all caregiving is done for the elderly. There are a lot of us that are caregivers for our young children. I have 2 boys with Duchenne Muscular Dystrophy that can’t do anything for themselves. My wife & I have to get them out of bed, give medications, feed them, take them to the bathroom & put them back in bed daily. The categories mentioned above we have to do them all daily or multiple times a day while maintaining our full time jobs. There is a whole community doing the same things we do when it comes to caregiving for the youth. It’s really frustrating when we have to travel for doctors appointments or even for vacation & all the wheelchair accessible rooms have only king beds with the assumption only elderly need wheelchair accessible hotel rooms. I would be happy to answer any questions or discuss any topics mentioned. I appreciate everything any caregiver has to endure because it can be really difficult at times.
Thank you, Terry. I’ve been gaining a deeper appreciation for the heavy workload and intricacies of caring for children with disabilities by listening to the podcast “Who Lives Like This?” hosted by Jason Lehmbeck and Elizabeth Aquino.
One question I have, inspired by the common themes yet extremely individual experiences I hear about (and have in my own life): If you worked with a designer on a worksheet to help a newly-diagnosed Duchenne Muscular Dystrophy family, do you think it could be useful for other health conditions? For example, other kids with progressive mobility challenges? Other parents who need to manage a rare and still-mysterious condition? Or do you think it would be most useful if you focused solely on DMD?
PS If anyone else wants to weigh in, please do. For example, Pete Wendel shared the particular challenge of dementia care in his comment. I wonder if some of the questions are more universally useful, too. And yet Pete’s dad being a “car guy” is a very specific challenge.
There are so many scenarios that involve caregiving. As a remote caregiver for my 88 yr old father with dementia and a parent of adult kids with brain health needs, I do have a few thoughts:
For my dad with dementia, it’s been tricky to try and have difficult conversations about the future. It’s so, so hard to process and accept a potential future reality without memory or the ability to keep key life skills (driving, going for long walks, and hunting & fishing).
Dementia Directives https://dementia-directive.org/
are planning sheets, similar to and end of life directive but focused on dementia. Sometimes it’s hard to have a conversation and having something to guide that talk, or reference in between conversations can be helpful.
It was helpful that they could be printed on paper & considered at a time where My dad could have some more control for when he was ready to process the information and reflect on it, making choices and prompting questions he had, so that he was in a better position to have a more direct and meaningful conversation with his caregiver/s.
Some things I’d like to find more help around for my dad’s situation:
The end of driving.
Given dad was getting lost while driving & demonstrated confusion and agitation at times while driving, I had to go about trying to get him to voluntarily stop driving. For a car guy, that was a non-starter. After numerous tries and conversations, I ended up having to write a letter to a geriatrician who then wrote a letter to the DMV which involuntarily revoked my dad’s driver’s license.
Know the process in your state for what’s necessary if you need to take action to keep a loved one safe (and ensure the safety of others) —Also, know anyone with good strategies and tips to make the transition easier? Ride sharing and taxi services in some areas address functional jobs-to-do. The gap here for car guy dad’s with dementia is an emotional job-to-do, giving up something you love doing more than most other things On this earth: driving his car & driving his car with people.
Thanks
Loving this discussion! Two items I’d add:
1. As a complement to someone to take notes at next doctor’s appointment, also give potentially needed help in preparing for next appointment with a list of key questions and issues to discuss.
2. Managing communication with others in M’s life. For some, M may want them in the loop. For others, he may not, but their inbound inquiries can be a stress that needs managing.
hi Susannah,
That’s really kind of you to be helping your older friend. I think you’ve already gotten a lot of great ideas from your community but in case it’s helpful: I did brainstorm a list of these when I developed my Helping Older Parents Course. The nine types of issues I see family caregivers having to work on are:
– Organizing support for daily life tasks (ADLs/IADLs)
– Addressing safety issues
– Addressing medical/health issues
– Addressing legal/financial issues
– Addressing housing issues
– Quality of life and helping the older person thrive
– Planning ahead (for health, care, finances, legal)
– Managing relationships and family dynamics
– Self-care
If you are wondering about the ordering of the list: it’s mostly in order of what people tend to ask me about first and less about what I think is more important to address first (although really, they are all important and they also almost all interact with each other).
I have an article explaining them in more depth here: https://betterhealthwhileaging.net/what-to-address-when-helping-older-parents/
Thanks for spearheading this conversation!
Thanks, Leslie! You are a fount of knowledge in this area. So appreciate your pointer to that article (everyone: give it a click) and that list. I see some overlap with what I came up with on my own (yay!) and some that I will need to add (even better).
As the care partner / caregiver you have to stay well also. I would add something in for the care partner, resources, a break, a place to find an ear or some peace or comfort that you are doing a good job or where you need to do different/more.
There was a mention of the patient/loved one’s mental and emotional well-being. I think that oo is important and finding space to reflect or what gives them joy and enabling them to express that to others.
Also – I recently completed a review of the top 20 pharma brand’s digital assets with a focus on caregiver/partner support and resources. The results are shocking – very few had good resources, many had none.
Thank you, Richard! Being a caregiver should have a diagnostic code if it doesn’t already — it can be a significant drag on your own health and ability to take care of yourself. Great reminder to add that to the requirements for our worksheet.
“What do you like to do? What brings you joy?” were among the first questions I asked M. In some ways it is easier for me to ask since I am not a daughter or grand-daughter who should, theoretically, know the answer.
Now that I think about it, I have shared back what brings ME joy, which includes, to M’s surprise, cleaning (as in dusting, vacuuming, doing the dishes when I visit).
We didn’t know these things about each other before we formalized our care relationship.
Hi Susannah, I’ve been a caregiver advocate for the past 6 years after caring for my husband through 9 unexpected surgeries. I was disappointed in the lack of empathy and coordination among the health care professionals and home care agencies. I ended up taking on my husband’s care myself. Previous replies hit on a lot of the same ideas I would have, but I would add two thoughts. One thing the surgeon found helpful was that I would take pictures of my husband’s wound so he could see the difference from week to week. Infections can be slow to show themselves, but the pictures really highlighted the difference – and I could email them to the surgeon eliminating the need for another lengthy car trip to his office. Also, I agree with you that diagnostic codes for caregivers are important. Here in Ontario, Canada, there is a code for doctors to speak with caregivers about their care recipient, but no code for talking to the caregiver about how they are coping. The patient’s doctor should end each call/visit with that question directed at the caregiver – away from the patient.
Cheers!
Carole Ann
Thank you, Carole Ann! Your advice is excellent and it’s great to know that you’re among the advocates creating change in Canada. Please know also that I caught my breath when I read “9 unexpected surgeries.” Holding space for a moment with you and your family as I absorb that number.
Thank you, Susannah. I hope to meet you at the Take on Tech conference (fingers crossed!) I’m helping Julie Drury and others to organize.