
On April 3, I was part of a symposium organized by Bryan Sivak, CTO, U.S. Department of Health and Human Services; Larry Smarr, Director, Calit2; and Gary Wolf, Director, Quantified Self Labs, where I presented the Pew Research Center’s findings on tracking for health. I uploaded my remarks in a separate post — this one is more of a “notes and impressions” download.
About 100 researchers, policy makers, designers, and toolmakers were invited and the only problem I had was that I wanted to talk to each and every one. I couldn’t sleep either night I was in San Diego because my brain was buzzing from the stimulation of so many geek-alikes in one place.
Joyce Lee was one heroic live-tweeter on the #qsph tag — you can check out her Storify for highlights. Maarten den Braber is another scribe to check out, since he brought a European perspective to an otherwise US-dominated event. Roni Zeiger‘s blog about Larry Smarr‘s presentation is a must-read: “I have the problem in my grasp.”
A few highlights from my own notes, following the Chatham House Rule (but if you said it and want to claim it, please let me know):
- Data can often power a discussion, not a diagnosis, and therefore a data-collection device or application should not need FDA approval.
- We need to keep in mind the challenges of representation in data sets, particularly if we want to use them for public health discussions. For example, RunKeeper has thousands of users in the Boston area, but none in Dorchester.
- Calculating one’s physiologic age vs. chronologic age is a measure of wellness and can be a very motivating vector.
- One institutional review board (aka IRB) recently changed their policy at the request of a researcher who wanted to return data to the study participants. That’s the good news. The bad news is that it is one of the oldest standing IRBs in the U.S. and no researcher at that institution had ever thought to give back to the patient community or include them in the research process before.
- Instead of handing a patient a prescription, how about handing them a decision tree? That is: Try X, but if you don’t see positive change within a week, try Y. If still no change, try Z.
- We need a “ForgetBit” — something that lets you update your FitBit data because you forgot to put the dang thing on before you went running, walking, etc.
- We are currently data-rich, but analysis-poor.
- Two very different views of contests and hackathons emerged: one clearly enthusiastic about them as a way to jumpstart a project or new thinking about a topic; another clearly skeptical, particularly if the project relates to big hairy (expensive) problems like global health or clinical trials.
 My personal self-tracking is minimal, but got supercharged thanks to Steve Zadig, a co-founder of Vital Connect, who put a Health Patch on me and a few other presenters in order to track our heart rate, respiratory rate, stress level, and a few other metrics during the day.
My personal self-tracking is minimal, but got supercharged thanks to Steve Zadig, a co-founder of Vital Connect, who put a Health Patch on me and a few other presenters in order to track our heart rate, respiratory rate, stress level, and a few other metrics during the day.
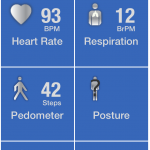 I’d just pounded a good, strong cup of coffee so I wasn’t surprised that my heart rate was high. I also felt a good kind of nervous about addressing this stellar crowd, so my stress level was also elevated.
I’d just pounded a good, strong cup of coffee so I wasn’t surprised that my heart rate was high. I also felt a good kind of nervous about addressing this stellar crowd, so my stress level was also elevated.
Once I took the stage, the app showed that my heart rate went up to about 150 BPM and my stress level stayed in the 90s except for two significant dips. I asked Steve and he said I probably paused to take a deep breath at each of those moments. I do remember thinking, “I’m talking too fast” and consciously slowing down — it was neat to see the data reflecting how my body was reacting to the stress and to my ameliorative pauses.
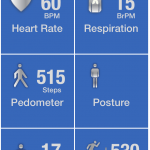 About an hour later, I checked in again and found that my heart rate had slowed considerably and my stress level had dropped way down. Steve Downs, who was also wearing a patch, showed me his read-out — stress level down to 1%! — so I sat there trying to breathe deeply and get mine down. Personal best: 4%. Steve is the Zen master of this round.
About an hour later, I checked in again and found that my heart rate had slowed considerably and my stress level had dropped way down. Steve Downs, who was also wearing a patch, showed me his read-out — stress level down to 1%! — so I sat there trying to breathe deeply and get mine down. Personal best: 4%. Steve is the Zen master of this round.
I stopped tracking it closely as the day went on but I’m pretty sure my stress level was at its lowest when I kicked off my shoes, rolled up my jeans, and watched the last rays of sun dip below the Pacific. Sand between toes = deep breath x 100 (approximate calculation).
If you have comments, questions, or observations, please share them below.
Insightful recap, thanks Susannah!
Thanks, Doug! My rubric is Be Useful and sharing notes from this meeting fits right in.
I’ve seen enough credits given to Bryan Sivak on Twitter for his great line that we are data-rich and analysis-poor that I may as well name him here. I’d love to hear what you (and others) think about this since it applies widely — to public health data, to personal health data, so-called big data, even survey data. There is a ton of data hiding in plain sight, waiting for someone to put it to use.
Here’s what I mean when I write that data is hiding in plain sight, waiting for good analysis to come along:
Charles Ornstein on the possible release tomorrow of “data on the services provided by – and money paid to – 880,000 health professionals who take care of patients in the Medicare Part B program.” Here’s his “get ready” guide:
http://healthjournalism.org/blog/2014/04/caution-in-order-when-tackling-newly-released-medicare-data/
Other examples of people who know how to ferret meaning from piles of data:
Fred Trotter
http://www.fredtrotter.com
My own organization’s blog, Fact Tank, releases a daily round-up of great data analysis. Here’s today’s:
http://www.pewresearch.org/fact-tank/2014/04/08/data-feed-a-decade-of-campaign-ads-gender-gaps-on-wages-and-jobs-outlook-for-global-growth/
And since we’re on the topic of both Pew Research and piles of data, check out all the data sets we publish for free:
Internet and tech
Latinos
Religion
Social Trends
U.S. Politics
Global Attitudes
News Coverage
Just catching up on this – I saw the post whiz by during heavy travel season. Now I have a large addition to my To Do heap. 🙂
> My rubric is Be Useful
Perfect: when someone asks me how to attract followers on social media, the first advice I give is “Say something useful.”
Love the article! Hope you don’t mind – what’s your view on physicians who are also trained as data scientists? Useful or unnecessary?
I think that’s a powerful combination. I’d love to see what someone like that came up with!
Just like we need physician scientists and physician creatives, we need physician data scientists. I suspect these are unicorns. For the patient facing practitioner, we need smart translational folks who understand what the data physicians conclude and can apply it in a way that serves the the patient and the system as a whole.
Interesting idea. Forces us to think…how much can a doctor really know?
Really happy to hear this. I’m finishing up my Pediatric pulmonary fellowship in a few months, and have been learning Python on the side to apply for the datascience program at Berkeley…and my attendings think I’m crazy! But with prevalence of digital health and biometric tracking skyrocketing, I’d like to be ready to interpret all that fast data from a medical standpoint, maybe even be able to personalize exercise prescriptions for my Fasthma patients. And yes, that is fat asthma. Thanks Susannah and Dr. Vartabedian for the comments, it helps to know that I’m not off my rocker.
We definitely need physicians trained as data scientists. Add nurses and other clinicians to that too! Now that would be wonderful.
I see two different comment threads above on the topic of “physicians as data scientists”. Rather than choose one or the other I’m going to start a new thread. Besides, this “comment” will probably evolve into a mini-blog post.
A while back I read an interesting article by Ciara Byrne on Why Doctors Make Great Object-Oriented Software Designers. The article focused primarily on a program at the company Modernizing Medicine, in which physicians are trained how to design and implement software that will help them in their specialties.
There is a reference to using data toward the end of the article:
Unfortunately, I can’t find much information on the program at the Modernizing Medicine web site, although there is a 2012 white paper on 5 Ways to Leverage Data-driven Patient Care [PDF].
Given the growing proliferation of Courses/Training on Data Mining, Analytics, and Data Science, it does not seem to require much of a stretch of the imagination to envision a short course / boot camp designed specifically for (and, ideally, with) physicians.
Perhaps a pilot data science for physicians tutorial might be proposed for either a data science conference or a medical conference. The Strata NY 2014 call for proposals is open until April 30. I’m not sure which medical conferences would offer conducive venues for this kind of thing. I’d be happy to work with anyone interested in exploring this trajectory.
Thanks, Joe! I love the idea of tutorials on data science being held at medical conferences.
Indeed, I’ll echo Sarah’s comment above about adding nurses and other clinicians to the target audience (not just physicians).
You may have seen me write about why I try to substitute “clinician” for the words “doctor” or “physician” whenever I can. It’s because of Lena Sorenson, who once stood up after a talk I gave at the Connected Health conference in Boston and gave such an eloquent and damning indictment of my use of the word “doctor” in my 7-word challenge to health care that I changed it permanently. (Original version: Recruit doctors. Let e-patients lead. Go mobile.)
Here’s the post I wrote about that event: Participatory Medicine, Connected Health.
Here’s the Boston Globe obit for Lena Sorenson if you want to learn more about her.
The videos for all the Quantified Self Public Health talks are now online:
http://quantifiedself.com/symposium/Symposium-2014/documentation.php
I think the QS and PH communities should manage a project to standardized machine readable health knowledge (i.e., quantify health literacy as function of age and sex) so its delivery can be near frictionless ubiquitious and just-in-time for digital citizens. Apparently, health literacy is not a universal thing according to the World Health Organization but I think it should be. The QS community enabled by commercial and Public Health interests have much to gain in terms of shifting the revenue streams and cost structure for being human by reforming the health knowledge structure (i.e., XMLizing it for machine readability) and its delivery channels and presentation layers. I could not find a comparison chart quantifying the differences in governmental definitions of health literacy and health education capacities / assumptions about pushing & pulling health knowledge as a function of age and sex. Personally, I am for democratizing digital human models that expecting parents tune upon discovery of their fetus. With the growing accessibility of 3D body surface scanners for frequent scanning and the eventual mapping of near-continous scalar data from wearables the stack of surface scans (i.e., curves, areas and or volumes), the perfect storm will occur in personal analytics when health knowledge is added to this reality system associated with the human from conception to postmortem disposition. Forget about interoperable Electronic Health/Medical Records! Providers’ inputs (i.e., biomedical imagery and measurements from regulated medical devices) remain important but appear minuscule contributions to one’s nDimensional Health Graph