As an anthropology major in college, I was required to take at least one course in archaeology. We studied burial mounds and earthworks (from afar, no digging) and it reminded me of Geology 101, when I learned how scientists spot patterns in the physical landscape. Geologists look for clues to the Earth’s past, and possible future, in the land. In the case of the linear earthworks of Illinois, my archaeology professor’s specialty, what was once a mystery is explained. Or rather, what was once obvious to one group of people (who built the mounds) is now explained (as best one can with limited evidence) to newcomers. The past is made visible as archaeologists gently probe and sift.
Now I use the metaphor of “internet geologist” to describe my work, sifting the evidence collected in surveys and fieldwork. The present is made visible, in data.
Caregivers are the latest group to come forward in our data, raising their hands to say, “Yes, in the past 12 months, I have provided unpaid care to an adult relative or friend 18 years or older to help them take care of themselves.” Or: “Yes, in the past 12 months, I have provided unpaid care to any child under the age of 18 because of a medical, behavioral, or other condition or disability.” A bit clumsy, aren’t they, these questions, these tools we use? But we dig on, hoping to find what we can.
Hmm, what’s this? 39% of U.S. adults now say yes to those two questions, compared with 30% in 2010? And those who do are more likely than others to say yes to nearly every other question in the survey, even when we hold other demographic variables constant?

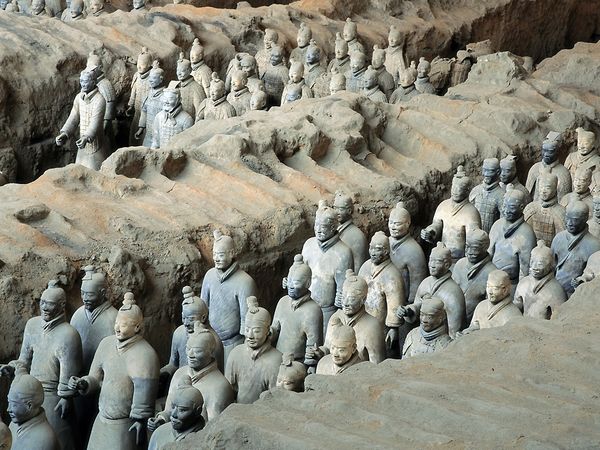
We had stumbled on the equivalent of a vast, underground army, each with a unique story, a unique role to play (please click through to the National Geographic story if you don’t know it).
But instead of terra cotta soldiers guarding an emperor’s mausoleum, we found flesh-and-blood caregivers guarding their loved one’s health. They answered question after question, yes, yes, no, yes, shaking off the dust of obscurity to show us where they stand today. Which is important, because it is where many of us will likely stand some day. Bedside. It is love made visible.
Just as archaeologists hope to learn from past civilizations, we hope to learn from present ones. What tools do these people use in their daily lives? Whom do they honor, by asking for advice and support? And, most importantly: Now that we know they are there, and growing in number, what are we going to do with this information?
Join me in this work, please, shining a light on your own story as a caregiver or listening as caregivers share.
Susannah, you are so right! I don’t know how it is in the States, but here with the lack of nursing staff, the uknown heroes of health care are all the wives. husbands, daughters, sons, sisters, brothers, aunts and friends who change shifts at the bedside of hospitalized patients. I know several who have spent innumerable days and nights at the bedside at the hospital, nursing home, or residence of seriously ill patients. If caring for a family member or a friend sounds natural, what can one say about all those volunteers who help alone patients to eat, who sit at the bedside and talk to them, who hold a hand… Health care could not exist without this army of silent, dedicated, uknown heroes…
It’s better here, but when someone in my family is in the hospital, we try to have a friend or family member stay with them. The people I’m most afraid for are those who are alone, without friends or family to look out for them.
Way late to the party but stumbled upon this. I am a geriatric care manager, and I’m at the hospital for my clients who do not have family, or have alienated their kinfolk. I wish my services were free.
Hi Jane! The conversation is never over – so happy you found us here. I wish your services were free, too. On my reading list today are two articles which illustrate why we need more people like you to look out for our fragile neighbors:
Health-care superusers overload hospital ERs (2014)
http://www.mcall.com/news/local/mc-lehigh-valley-hotspot-20141101-story.html#page=1
If this was a pill, you’d do anything to get it (2013)
http://www.washingtonpost.com/blogs/wonkblog/wp/2013/04/28/if-this-was-a-pill-youd-do-anything-to-get-it/
Great analogies. Lighting up dark information is one of the great challenges of health care today, making the invisible visible, then harnessing or acting on the new info. Its an emerging skill that has much to learn from open communities. Not only does the new info need to be found, made available, filtered and distributed, it needs the evolution of a community that can put it to work, to influence decisions and policy and create value. One of the great tasks of our time. Great work!
Thanks! I’m sure you saw this article about home visits by trained nurses, but just in case you didn’t:
If this was a pill, you’d do anything to get it, by Ezra Klein (WaPo, 4/28/13)
It reminded me of your brilliant insight that the “blockbuster drug of the century: an engaged patient.” I wonder if you’d help come up with an equally catchy tagline for the power of caregivers? You know, in your spare time 😉
I liked Leonard’s comment on caregivers — the “invisible economy of love.” As you may recall, we’re working on the Health Rosetta Principles (fka “95 Theses for a New Health Ecosystem”). I riffed off the Rosetta theme with my company name — Rosetium. If you go to the website, you’ll see I refer to it as “Healthcare’s Missing Element” (as in an element in a periodic table). If you decode element “143”, that is SMS for “I love you” (1 letter, 4 letters, 3 letters). The intent is that love is the missing element. We know how important that is for caregivers but I also see it in the best examples of companies adhering to the Health Rosetta. They focus on the Quadruple Aim — by loving their team and creating a great care team experience. In turn, that naturally leads to an improved patient experience. That facilitates the “magic” — i.e., a great partnership between the professional and non-professional members of the care team (including the patient, of course). That naturally leads to improved outcomes. In the right model, that leads to lower costs.
Further riffing off of the Rosetta theme, the archetype I used in my TED-style talk and the documentary I’m working on is “Rosie”. She’s the bedrock of our healthcare “system” as the female head of household or what I call the “Family Chief Health & Wellness Officer”. Rosie is key to addressing the wildly under-performing healthcare estatus quo that has become, in my opinion, the single greatest immediate threat to America. The documentary is meant to activate the “Rosie’s” who can help restore the American Dream that healthcare has devastated (just look at what has happened to the Middle Class due to hc costs). “Rosie the Riveter symbolized America pulling together during WWII. I hope “Rosie the Restorer” will do the same as the status quo threatens America every bit as much as any foreign power. I’ll drop you an email with my 12 year old son’s artistic rendition of Rosie.
Susannah, this is a wonderfully written piece bringing much needed attention to the rapidly growing caregiver population. As an anesthesiologist, I often overlooked the important role these individuals play in the management, both physical and emotional, of every one of my patients. It wasn’t until I became a caregiver myself, did I fully comprehend (and fully appreciate) the role of these selfless, loving, and caring people. I never imagined becoming a caregiver to my wife at the young age of 33, but when Molly was diagnosed with breast cancer in 2011, I transitioned from “professional caregiver” to a personal caregiver. I felt completely unprepared for the journey, but the experience transformed me. I listen more. I judge less. I set aside time more for my family above all else. I am a better physician now. I am a better husband and father. And I am a better person.
I agree with you that it is important for everyone to share their story. Here is mine: https://www.consano.org/blog/single/18-the-most-difficult-patient
Amazing, amazing, amazing. I’ve read that post twice now and I’ll read it a third time, it’s so good. Thank you for sharing it.
Thank you so much, Susannah. I really appreciate your kind words. This essay was such a difficult thing to write and share, but the response I’ve received has made it so worthwhile. I am glad that others can learn from my story, and I have been amazed at how many other people have felt the same way as I did.
I look forward to meeting you at MedX in September. I signed up for your master class and I’ll also be giving a presentation about the first six months of Consano, the nonprofit crowd funding website my wife and I started after her journey through breast cancer.
Wonderful! I’m so glad you’ll be part of the class. Can’t *wait* to meet and learn from you.
My wife is a cancer survivor who also has multiple sclerosis and other chronic conditions. I can relate to feelings of helplessness, and the need to channel fear down alternative pathways (including repression), expressed here and in your blog post.
I am heartened to read of the way this challenging journey has enhanced your empathy and presence with and for your patients and those who care for them. In my own journey, I find being empathetic, present and compassionate – with my wife and others – to be an ongoing challenge.
Family caregivers – a recipient’s perspective: This will be a rather lengthy but I hope worthwhile story. It happened at a time when there was no internet and very few relevant information options.
In 1995 I had hip replacement surgery. The surgery went well but I happened to be in the hospital over the July 4th holiday weekend. During that weekend something went drastically wrong – and in the absence of a senior authority what was done cost me two years of my life and my wife one of her most challenging experiences.
On July 2, 1995 at 2:00 PM I started bleeding internally in the area of the new prosthesis causing a great deal of pain. I didn’t know at the time I was bleeding. When I complained the only thing the staff could think of was to do an X-Ray to determine if my hip was dislocated. It was not. By the next day the pain was more intense and now they discovered by red count was low. Rather than address the issue they started giving me units of blood; and over the course of 3 days I received 12 units of blood. When my surgeon came back on the 5th of July and took a look at me he brought me immediately back to the operating room. I came out of surgery with no prosthesis and multiple antibiotic resistant infections.
At that time a person had to be infection free to at least 12 months before a prosthesis could be replaced. However, I was discharged with a ‘pic’ line and told that arrangements would have to be made for public health nurses to do home visits to oversee care. There were three issues: 1) eliminate infection through powerful IV antibiotics; 2) wound care; and, 3) taking care of the rest of me. They had to leave a wound open from the outside of my right hip into the inner joint. Each day required wound care that included packing antibiotic laced gauze into the wound until it healed from the inside out.
Now it gets even more interesting. Because of my insurance I was only eligible for 2 weeks of specialized home care; so at the end of that time my wife had to be shown how to take care of my wound and apply the IV antibiotics; and of course take care of all the others things that I needed in terms of support. My wife is not a nurse; had no experience; but was as brave a person as you can imagine. It took seven months of progressively more powerful antibiotics to rid me of infection and for the wound to heal. I spent the entire time in a hospital bed in our bedroom with my wife displace to a couch. She had to handle biologic waste that no one untrained should be asked to to. Then I spent the next 13 months in a wheelchair because I had no hip at all on my right side. Finally in September 1997 I had a replacement prosthesis put into my hip.
This is not the end of the story but it is the end of the current narrative. There are many things wrong with our health system, but no untrained person should be expected to do what professionals are trained to do – no matter how straightforward it is to the professionals. To have a willing caregiver is a wonderful illustration of the strength possible in relationships. However, not only is it difficult for the caregiver, it is agony for the recipient of care to see a loved one have to deal with these issues. Thank you Barbara.
Thank you for sharing your story! I’m floored by the tasks your wife was asked to take on. What if she hadn’t been able to handle it? I shudder to think. Very brave woman indeed.
Thank you Susannah. She truly is brave and very strong. I’m guessing that these are characteristics of many of the caregivers you’ve been writing about. Thanks for creating the circumstances that allow these issues to be brought out so clearly.
See my latest post about team dialogue while caring for our son http://wp.me/s2CyvO-dialogue
Danny, I’m in tears over breakfast, reading your post. Sad for you and your family, happy for the gift of life and love, hopeful for the future tears. Thank you for sharing it.
Hello Ms Fox,
Enjoy and always look forward to your PEW info, data and statistics. You all do great work.
You article and analogy rings so true. Caregiving is in crisis as the sandwich generation and senior population swells and grows.
Sandwich generation families and caregivers are truly silent heroes and needs more support, resources, information and insights. As once a former certified nursing assistant (CNA), now a geriatric PharmD who happens to care for young children and aging dad, I truly sympathisize with family caregivers.
As a pharmacist, I can help dad, grand parents with medication management, pill box fills, charts, apps, etc. I know what questions to ask the MD and cordinate care but our health care system is so complex health care professionals still find it difficult to navigate. For those who are not equiped with knowledge and tools, it hard, difficult and quite overwhelming.
I am working with Carenovate (http://www.carenovatemag.com), an educational platform with a focus on providing caregiving insights, health and medication literacy for caregivers. We have compiled a quick, 5 question survey designed to help us understand how and what resources family caregivers needs when it comes to helping loved one manage & coordinate everything including medications/medicines. Feel free to share with your networks Caregivers & Medication Management Survey: http://ow.ly/kgRHU
Continue the wonderful work and feel free to reach out to us info@carenovate.com if you need a clinical pharmacist who happens to be a caregiver – family and professionally
Dr Ero
hmm, looks like last comment didn’t go up, so I’ll test here…
Not sure why, but was not able to post another comment (maybe too long?) so I’ve posted it here:
https://www.evernote.com/shard/s4/sh/fa013111-6237-4247-b3ed-3e558050ae43/f1caf0771c9879832c3bfc09d4a9e7e2
Thank you! Sorry about having trouble with comments. Because of spam, I have to approve every one by hand, so there is sometimes a delay. But I don’t see the one you must have drafted and lost — glad you saved a copy.
Everyone — check it out. Leonard knows what’s up.
Made my day. I hope you don’t mind if I quote you in my bio with that last sentence. #seriously
The issue does seem to be something about the length of the comment, these ones seem ok.
I enjoyed your comment … and suspect that it did not appear in Susannah’s moderation queue due to the number of links rather than its length.
Over the past few years, I have moderated my commenting frequency & style in response to the moderation imposed by many automatic comment filters, and try to restrict the # of links I post to 2 (or at most 3).
Thanks for the tip, Joe! A case of comments made invisible. 😉
Thank you so much for this report. I often say that my caregiving and advocacy for my son Case would be vastly different and, I fear, much less comprehensive, were it not for mobile technology. I do wonder about the “next level,” as it were, and if and how caregivers can push it to that. To me, that next level is comprehensive mobile medical records. For now, I request and scan Case’s records every 6 months or so and have them on Dropbox in folders by medical speciality. That process, however, is burdensome, unsearchable, and incomplete given I still can’t load imaging like MRIs. Thoughts?
An inspiring post and comments (as usual). I was delighted to learn more about your background and motivations … and can better appreciate your propensity to unearth interesting insights, both in your surveys and the comments you elicit on your blog posts.
Your emphasis in this post on the variations of making the invisible visible remind me of another friend’s insights into discussing undiscussables. Earlier today, you tweeted a link to a blog post by a woman who wrote about her guilt regarding “not working hard enough” to control her diabetes. In a comment here (and post elsewhere), Scott Finkelstein wrote about his feelings of helplessness, fear and anxiety about his wife’s cancer.
I would never diminish the challenges faced by them or any others who are willing and able to discuss their chronic conditions – or those experienced by their loved ones – publicly or privately, but I do believe there is therapeutic value in being able to discuss health challenges. I also believe there is another vast, underground population – I would not call it an army, as that would imply cohesion, camaraderie and mutual awareness and support – that is experiencing chronic conditions that they are unwilling and/or unable to discuss … which adds another layer of complications to their health challenges … and the challenges faced by those who care for them.
I don’t know whether or how the unspeakable challenges faced by such people can be effectively unearthed. I’m sure many are already represented in your Caregivers report and other prior reports. But I suspect an experienced Internet geologist might be able to uncover new insights into the dark, shadowy realm experienced by those with undiscussable health challenges.
Joe, I read your comment the minute it came in but just now had a moment to click through and read the “undiscussables” post. That’s a keeper.
Everyone: check it out. Bonus points if you can help me identify more “undiscussable” topics related to caregivers. Some were identified in a lively #eldercare Twitter chat today, too. Here’s the transcript:
http://www.symplur.com/healthcare-hashtags/eldercarechat/
I find it challenging to identify the signals in any Twitter chat [transcript], so I don’t know if any of the following was already chatted about there, but here are a few thoughts.
Brene Brown’s most recent book, Daring Greatly: How the Courage to be Vulnerable Transforms the Way we Live, Love, Parent and Lead, includes a chapter on The Vulnerability Armory, which includes a section on Daring Greatly: Clarifying Intentions, Setting Boundaries and Cultivating Connection, that I believe is relevant to undiscussable topics for health caregivers (healthcare givers?).
Much of the book highlights the many rewards that are often enjoyed by those who embrace and practice vulnerability, but this particular section addresses some of the risks. Brene notes that she includes many stories about herself and her family in her books and other channels for sharing her work (e.g., her amazing TED talks). But here she says “I don’t tell stories or share them with the public until I’ve worked through them with the people that I love.”
I think it is particularly important that caregivers be sensitive to the vulnerabilities of those they care for. There seems to be a growing awareness of possible negative side effects from parents who are “oversharing” photos and stories of their children on Facebook. I can imagine that oversharing by those who care for elderly parents or other relatives may also be[come] an awareness issue.
Your report suggests that the vulnerability of loved ones has a strong boosting effect on the solitary act of healthcare information seeking, but I suspect there are significant differences in boosting vs.dampening effects on the seeking of community and connection – outside of anonymous online forums – depending on the source of the vulnerabilities.
As for “undiscussable” topics, I would include any kind of condition that has social stigma or involves symptoms that are uncomfortable topics of conversation, such as mental illness, sexually transmitted diseases and at least some variants of IBS.
Hi Susannah, just re-read your important post. Proud to be in the army of caregivers. Thank you all for your work. The longevity of care and new tools around us are changing our world. Keep shedding light on this important arena; I have to trust it will help individuals and change communication and policy.
I keep coming back to the idea you raised about archaeology and data. Writing a post where I’ll quote you. I think you’re right and it makes data journalism really different than other kinds of journalism, if you can call it that, in 24-7 culture. Data stories take a long time to mature, but the pieces of evidence that come out can feed the story for years.