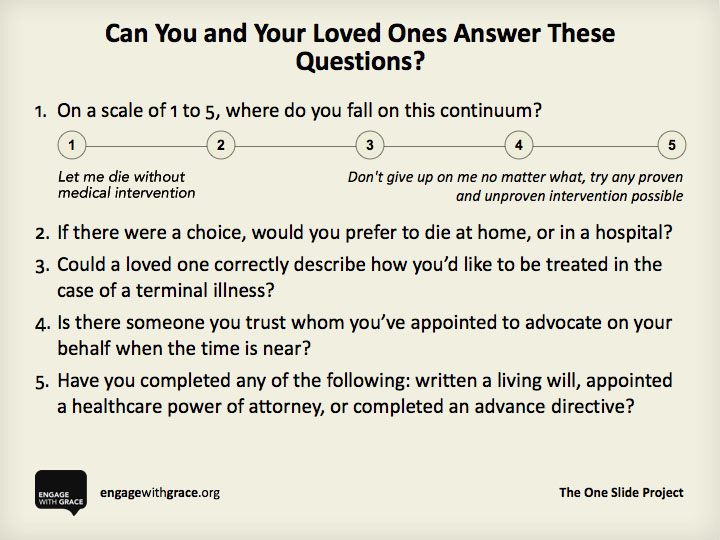
Can you and your loved ones answer these questions?
1. On a scale of 1 to 5, where do you fall on this continuum: 1 = Let me die without medical intervention; 5 = Don’t give up on me no matter what, try any proven and unproven intervention possible.
2. If there were a choice, would you prefer to die at home, or in a hospital?
3. Could a loved one correctly describe how you’d like to be treated in the case of a terminal illness?
4. Is there someone you trust whom you’ve appointed to advocate on your behalf when the time is near?
5. Have you completed any of the following: written a living will, appointed a health care power of attorney, or completed an advance directive?
This Thanksgiving holiday, consider printing out this one slide and leaving it on a table or countertop where your loved ones will see it. If they want to engage with the questions, be ready for a meaningful conversation about the end of life.
I used these questions as an intimacy hack, a way to jump up a few levels in my relationship with my elder cousin, M., when he asked me to be his caregiver and health care proxy. We needed to transform ourselves from fond friends to trusted partners. I needed to know what he wanted so I could fight for it, at the end.
Happily, he was in good health when we had that first conversation. We went on to talk about his plans for attending the opera, for hosting more dinner parties, and other favorite activities. Death was not the centerpiece, but it was on the table that day. It had to be, as a symbol of how serious we both were about this new stage of our shared journey. Because I believe that one of greatest gifts you can give to a loved one is to ask them what they want at the end of life and then to try to get that for them.
Please share your own experiences with end of life planning. And if you use the Engage with Grace questions, let me know how that goes.
Yeah I have a living well (that’s worthless). On top of the long COVID I have crohn’s. I have been resectioned a good half dozen times already and have some good insidee parts lying in landfills. I had a standing order that if something happens requiring to put the bag back on to let me go and created the living well with those wishes. Wasn’t the bag as much as all the complications I had from it. My wishes were clear to my mother, the babe and my surgeon. Wound up in the ER with what I thought was another intestinal blockage, but turned out it was a twisted bowel. My surgeon was called and rushed over. And knowing my wishes, they conspired to get me to sign the release. They hit me with heavy drugs and cried and wore me down where I signed off. I would have went out on top and very happy. I had it all but since (10 years now) I’ve struggled and been in hell pretty much. I don’t blame them or act insufferably over it but it’s been a really tough decade.
Mark, thank you for sharing your perspective and you have my sympathies. We can only hope that people we trust will believe us when we express our wishes, and do their best to follow our plans, not theirs.
Thanks. Can’t be mad that ppl didn’t want to see me die. I know better but I know because I know and I just know aren’t reasons others accept in these instances. I know I’m still here because I have to be but I don’t have to be happy about it lol. I still believe in all things possible so however unlikely, there’s a chance things will improve. Would love to get rid of the long covid issues to work on the other stuff tho.
I almost forgot about this, Susannah. It’s a tradition as old as the blogosphere. Thanks for reminding me. I hope you have a relaxing day.
Thanks, Bryan! Chaos on Twitter has centered me on what I want to do with whatever platforms I continue to use: To be useful. Back to basics. Like sharing this old chestnut around Thanksgiving each year.
I’ve completed an advanced directive but ti is surprisingly difficult to know what to do with it now that I have it. Every NHS doctor and nurse I have asked about this and palliative care have told me that it’s too early to talk about this stuff. Still, my wife has all the details and has medical power of attorney.
The most difficult bit: I’d like to die at home but my wife is worried that she won’t be able to cope. I’d like to give her permission to send me to hospice if she finds it too difficult but finding the right words for this is so hard (to say the least).
I’d love to hear from experienced caregivers, hospice nurses, palliative care experts, and others about whether it is ever “too early” to talk about what you want at the end of life. Maybe the clinicians you’re talking with are uncomfortable with your clarity.
As I wrote in the post, I introduced the topic of end-of-life when my elder cousin was in great health — bicycling to Quaker meeting on Sunday, for example — and death was not on the horizon except for the fact that he was in his 80s (but his siblings were — and are — still alive and in their 90s now).
I only have limited experience with death at home, but I can say that it did take a lot of work to set up the house to be comfortable and to get all the supplies we needed, but then it was a glide path toward infinity.
Hello again Susannah – I love this site, and your writing, and this special topic. Before my heart attack provided me with a much-too-early forced retirement, I spent the last years of my long public relations career working in hospice palliative care alongside my physician and nurse colleagues on a 17-bed in-patient unit at our regional hospital. It was a wonderful life-altering experience. As one of our senior nurses used to say when people asked her if working with the dying was depressing: “This care is about living, not about dying…” I learned so much from my colleagues, but mostly from our patients and their families.
I updated my will and Advance Directive and a new form I completed along with my GP called M.O.S.T. (Medical Orders for Scope of Treatment – which gets updated once a year in case my health or my preferences change). This was in my 50s right after my heart attack – it’s never too early to plan ahead when you live with a chronic and progressive condition. Statistically, I have some idea how I’m going to die someday – but let’s face it, I could get hit by a bus tomorrow when I least expect it!
But my experience working in end-of-life care taught me something that I was surprised to learn about the question “Would you prefer to die at home or in a hospital?” I used to think that OF COURSE most people would prefer to die at home if possible. Who wouldn’t want to be around familiar surroundings and loving relatives gathered around their bedside as they peacefully drift off, hands gracefully folded over the embroidered coverlet?
But something to consider seriously before people insist they want to die at home – as Kevin’s wife rightly worries about (above) – is the realistic capacity of the family caregiver to provide 24/7 care that dying patients may ultimately need at home. This is especially important when the dying person is a frail elderly patient, and the person providing the care is most likely their frail elderly spouse – the kind of caregivers who could use a caregiver themselves.
Without close family or expensive home nursing assistance every day and every night, the exhausted frail elderly spouse is often run ragged trying to run a 24/7 household while responsible for all personal care for the patient. The frail elderly spouse is responsible for organizing and administering drugs, bathing, feeding, changing dressings and diapers. And when the patient falls out of bed in the middle of the night, it’s the frail elderly spouse who will struggle in vain to rescue them.
Family members who promise that a dying person will die at home often feel guilty about admitting they can no longer cope with caregiving any longer. We’ve witnessed family caregivers who felt horrific guilt because they had to break their promise to the patient – by then at great cost to the spouse’s own health.
It is never too early to plan ahead – ideally as in M’s case, when the patient is in “great health”.
Thank you for this, Susannah. . .
C.
Carolyn, thank you for this generous & detailed advice. It really is never too early to plan ahead.