My dad was a survivor — of a heart attack in his 50s, kidney cancer in his 60s, and an initial diagnosis of melanoma in his 70s. Melanoma recurrence and complications of treatment are what finally got him.
A lifelong runner, Dad kept meticulous notes about his mileage and heart rate on paper. He bought three pairs of sneakers at a time so he could rotate their use, carefully marking them so they would wear out evenly. Each time Dad was hospitalized, my mom, a journalist and master caregiver, took over as record-keeper. Thanks to her tracking of symptoms and treatments, Dad avoided countless medical errors as we moved between three care facilities that last year of his life. My mom does not appear on any health care organizational chart and yet she saved the system an enormous amount of money.
We tapped every resource we had in our pursuit of Dad’s well-being, from the comforts that money can buy to those afforded only by presence and prayer. We left it all on the field in 2017.
Now when I hear about someone else caring for a loved one or starting a steep health journey, my heart aches to give them advice. But I worry. Will it be welcome? Will they be able to afford the time we spent? If they are not now part of a faith tradition or in the habit of self-tracking, what good is our advice to pray or take notes? When I suggest a palliative care consult, will they hear “death is near” instead of “soothe that itchy rash”?
I worry that I’m like those busybodies who had opinions about how I was feeding/dressing/raising my children. No, no, and no, thank you.
So I collect evidence just in case I get the chance to share it:
- For hands-on care and frequent visits, whether it’s you or someone you hire. Read: “If this was a pill, you’d do anything to get it” by Ezra Klein (Washington Post, 2013).
- For kicking the tires on a clinical trial before you enroll. Read: “Clinical Trials: What Patients Need to Know” (FDA); “What you need to know about clinical trials (before you need one)” by Alison Bateman-House, MPH, PhD (Forbes, 2017).
- For symptom tracking, whether you are part of a clinical trial or not. Read: “For some cancer patients, monitoring symptoms can extend their lives,” by Stephen Ornes (Washington Post, 2019) and “Overall Survival Results of a Trial Assessing Patient-Reported Outcomes for Symptom Monitoring During Routine Cancer Treatment,” by Ethan Basch, MD, MSc; Allison M. Deal, MS; Amylou C. Dueck, PhD, et al (JAMA, 2017).
- For palliative care to start as soon as medical care ramps up. Read: “Palliative care: Sooner may be better” (Harvard Health, 2011).
- For connecting with peers, whether you are a caregiver or a patient. Listen to: “Interview with Terry Langbaum and Dr. Tom Smith on issues faced by long-term survivors with metastatic cancer” (New England Journal of Medicine podcast, 2019). Watch: “Peer to peer health advice” (Reframe Health and Susannah Fox, 2017).
- For dying where you are comfortable. Read: “Is dying at home overrated?” by Richard Leiter, MD (New York Times, 2019).
Now it’s your turn. What advice do you long to give to someone newly diagnosed with your condition or in a caregiver situation like yours? What articles and evidence do you keep in a file, in case someone ever asks?
Comments are open. Please share!
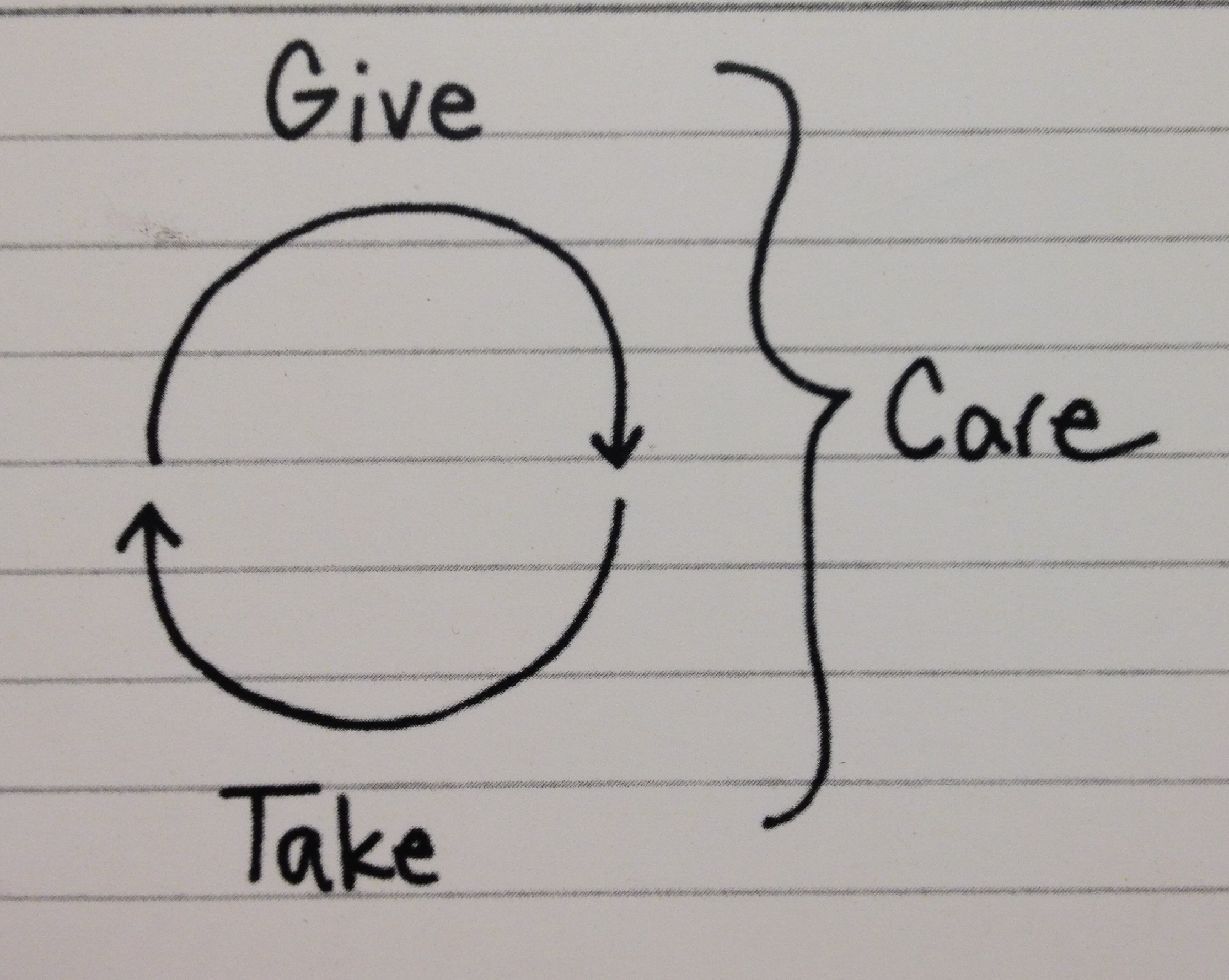
Image: Give – Take – Care, by Jessica Hagy.
For Susannah’s readers/followers: I’m a layperson turned end-of-life (EOL) reform advocate and author. My family’s experiences of each of my parents’ unexpected terminal hospitalizations was bitter (2004/05…not too much has changed since then) despite the folks’ advance planning, such as we knew to do it. I undertook to get to the bottom of all the failures—the family’s, my own, the system’s. I authored two books and arrived over time at an EOL lexicon…a series of understandings, insights, and assessments. I focus on an aspect of the scene that most people, even “death-positive” and “death-literate” tend to, and do, avoid. I’ve taken a straight-on look at why, and how, exactly, we end up ensnared in overmedicalized dying situations that we say, or even vow, we want to avoid. So, I recommend reading my two books, in reverse order. They are:
• The Promised Landing: A Gateway to Peaceful Dying
• Notes from the Waiting Room: Managing a Loved One’s End-of-Life Hospitalization
As I am the indie publisher as well, you may find them first at my site, http://www.AxiomAction.com and next of course, on Amazon and world-wide by order at bookstores.
For a quick overview, see my two journal articles, both freely available:
– 2019’s Understanding Demises as Destinations Across Our Dying Territory, https://cdn.ymaws.com/www.csa.us/resource/resmgr/docs/journals/journal_76/Windrum.pdf
– 2013’s It’s Time to Account for Medical Error in “Top Ten Causes of Death” Charts,
https://participatorymedicine.org/journal/opinion/commentary/2013/04/24/it’s-time-to-account-for-medical-error-in-“top-ten-causes-of-death-charts/
All this work goes well beyond current guidance from medicine (conversations, directives, and proxies) and civilians (conversations, spiritual elevation to support equanimity and resolve).
May I boldly say here that Susannah has endorsed The Promised Landing; her comment closes the list of “blurbs” appearing on TPL’s rear cover.
Be well.
Thank you, Bart! You went through a terrible thing (twice!) and have channeled your energy toward improving the journey for others. What a gift to the rest of us.
Thank you all for the amazing resources we can use or bookmark in time of need for ourselves and for others!
In addition to navigating the system, coordinating care, and avoiding medical errors, another big challenge that patients and families face as during any illness (serious or not) is knowing how to have a voice in their medical care decisions.
While we all agree that we should all advocate for ourselves…knowing HOW to advocate has never been well-defined. What does the behavior actually entail? What are the steps to having a mutual partnership with a physician/clinician in the absence of having the same degree of medical expertise? What does it mean to have a medical treatment plan that is designed to align with your personal preferences, priorities and values?
I published “Healthcare Choices: 5 Steps To Getting The Medical Care You Want And Need” (Rowman & Littlefield, 2017) to lay out a process (the “CARES Model”) that people can learn and apply to any medical condition/situation. In the book, Chapter 5, specifically discusses how readers can use the CARES Model to have a voice in aging and end of life decisions. It’s available on Amazon: https://amzn.to/2X7u0NC
I appreciate your work,
Best,
Archelle Georgiou, MD
Wonderful recommendation – thank you!
People, please don’t be shy about sharing resources that YOU have created (as Bart and Archelle have done) or resources that you keep in a file (virtual or real).
Susannah, as always, I am grateful for your intellect and your heart! Thank you for sharing this. Here’s what I wish–after watching my father die from lung cancer when I was 14 and facing now my mother’s long slow decline at the age of 86–I wish I had a magic guide, not just for all the things you mention here, but how to manage the fraught family dynamics that are an inherent part of any protracted caregiving experience, even in the most functional of families (mine is NOT in that category). How do we emerge on the other side as unscathed as possible? (I am aware as I write that may sound selfish.)
Beth, your question is not selfish and you are not alone in asking it. Every family is different, which is why giving or getting advice about sensitive situations is so difficult. One weekly newsletter I receive (and almost always read – a high compliment) is from AgingCare.com. Often, I admit, I open it to experience a bit of Schadenfreude, as in “whew! That is a terrible situation – glad it’s not me.” Other times there is a Q&A or article that seems targeted directly at me, at that moment.
For example, my siblings and I take on different roles and sometimes I feel like my portion of work is bigger than theirs. I felt resentment building inside and, remembering an article I’d read about sharing your feeling with your siblings (or other co-caregivers), I let my brother and sister know how I felt. To my surprise and delight they immediately said “you are right, we need to do more and, if we can’t, please know that we see your work and really appreciate it.” Being seen and appreciated lifted a significant burden of resentment off of me.
If people know of other resources, please share! (And btw, gently counseling people – including oneself – to seek therapy is also a fabulous path.)
Oh my goodness – thank you, subscribing now. Also, yes, therapy. Thanks for reminding me to remind myself. 🙂
Thank you, Susannah, for asking and aggregating great resources for those who may be in need of some “advice”. As parent and a health care professional, I was totally unprepared for my son’s terminal illness diagnosis and his decline leading to his death at age 14 (not that anyone can be prepared for this). At that time (2001) there were very limited online resources for a family like ours. Since then, a wonderful resource has become available, started by a mom (Blyth Lord) who had navigated her own daughter’s illness and death, CourageousParentsNetwork.org What I love about the network is that is peer to peer support when one is ready and when one needs it.
Pam
Pam, you can’t see me but I’m bowing to you, with thanks.
Your description of the network that is there “when one is ready and when one needs it” is so beautiful. I imagine a hand reaching out and catching mine as I reach for it in the dark, a force steadying me at the moment I stumble, a net that appears underneath me at the moment I fall from the trapeze.
I ask if they know about Integrative and Functional Medicine. To treat root causes of diseases when possible. Many still have not heard of either. But they’d like to to the bottom of things.
Thanks, Jean! If you could share 1-3 articles that make your case, what would they be?
Example of the Functional Medicine approach:
Functional Medicine has said for years that inflammatory foods are linked to depression, anxiety and more. This podcast interview with Dr. Daniel Amen addresses this. https://drhyman.com/blog/2019/11/06/podcast-ep79/
Dr. Amen says how strange it is that “… past methods of treating mental health disorders didn’t actually look at what was happening inside the brain”.
But looking at brain health should be the first step, even before psychotherapy or counseling.
Anti-inflammatory foods, exercise, social supports are common Functional Med treatments for brain health. Meds-first treatment is reserved for bipolar and schizophrenia, gaining time to look for root causes.
Psychology Today now reports that anti-inflammatories can help. But again, what about root causes? Well, you can patent anti-inflammatories, not anti-inflammatory foods. To me, that says it all.
https://www.psychologytoday.com/us/blog/expressive-trauma-integration/201911/anti-inflammatories-help-major-depression
Thanks, Jean! These are great resources to dig into.
An additional free resource: CaringBridge.com is extraordinary. The site was developed 25 years ago to help streamline communication with friends and family about what was going on with a loved one. The benefits of journaling extend beyond efficiency. Sharing the journey is a healthy way to process and express emotion. And the community who loves you better understand how to engage and support you.
A thousand times yes: “the community who loves you better understand how to engage and support you.”
Big respect for CaringBridge for creating one of the first platforms for people to make the jump from “I wish I could help” to “I’ll pick up David from school today for you.”
Hello,
The record-keeper part of this post really caught my attention. I am that person. Our 90 yr old parents are now in a care home with full-on dementia and receiving great care. The 3 year road to here though included much learning, monitoring the degradation of health, many doctors visits, hospitals…
I was trying to find a place to keep this info so my brother (N Carolina) my sister (British Columbia) and me could stay updated. I built an online workspace and organized the info there, sharing the workspace with Ruth and Ron so they could login and be always updated as we traded off being with mom n dad.
I’m about 1/2 way through developing http://simplifycaring.com. The public side is up and says what we want to do and the back-end is coming along well. It is essentially an eldercare organizer where you can post photos, keep track of financials, Dr notes, build lists like funeral arrangements and schedule everything.
The goal of the online tool is to encourage MORE engagement with care giving and including family and other carers as much as you like. If there is peace of mind that your info is organized and readily accessible and secure, I think it helps us focus more on the loved one we’re caring for.
Anyway, I’m rambling now. Thank you again for this post.
Rudy, thank you so much for adding your voice to this conversation and sparking a couple of new thoughts.
First, I love that you are building a tool to solve your and your own family’s problems. We need more of that in health care — actual patients & carers contributing to the solutions.
Second, I wrote this post to gather up evidence for what I “know.” Instead of relying on my own anecdotal, personal experience, though, I wanted to see what I could find that “proves” the worth of the advice I want to give. It turned out to be harder than I thought, particularly in the area I care the most about: peer to peer connection. There’s a ton of evidence showing that people are engaging in peer health advice, but not much that I could find related to evidence that it WORKS (i.e., resolves a symptom without further intervention, saves them money, prevents a medical error…all of which I have seen in my own life among peer patients and carers.)
If you or others are interested in how that evidence might be gathered, check out this new viewpoint published in the Journal of Medical Internet Research: A Call for a Public Health Agenda for Social Media Research by Pagato, Waring, and Xu.
Having had dad undergo heart surgery and a few years later diagnosed with Prostate Cancer and a mum with Breast Cancer I know only too well the challenges of taking care of being involved in a loved ones care. As a business owner we have been fortunate enough to work with a leading Cancer Hospital in Melbourne Australia on an app called ‘Second Ears’. The app aims helps patients to record consultations, take notes and securely share them with their partner or others in their care team. This enables them to be more empowered, better understand and participate in their treatment. We know that more engaged patients get better health outcomes. A few details about the app are here: https://wavedigital.com.au/folio/peter-mac-cancer-centre-second-ears-app/
The app has successfully completed a pilot and will hopefully be released for use later this year.