Continuing my series of stories that hopefully make you say, “Wow! How did they come up with that?”
Sara Riggare has been living with early-onset Parkinson’s disease since she was a teenager. In my book, Rebel Health, I wrote about her as an example of a Seeker, Networker, and Solver. She is constantly on the hunt for information. She pools resources for herself and her community. She conducts personal science experiments to optimize her health and she adapts assistive devices to meet her needs.
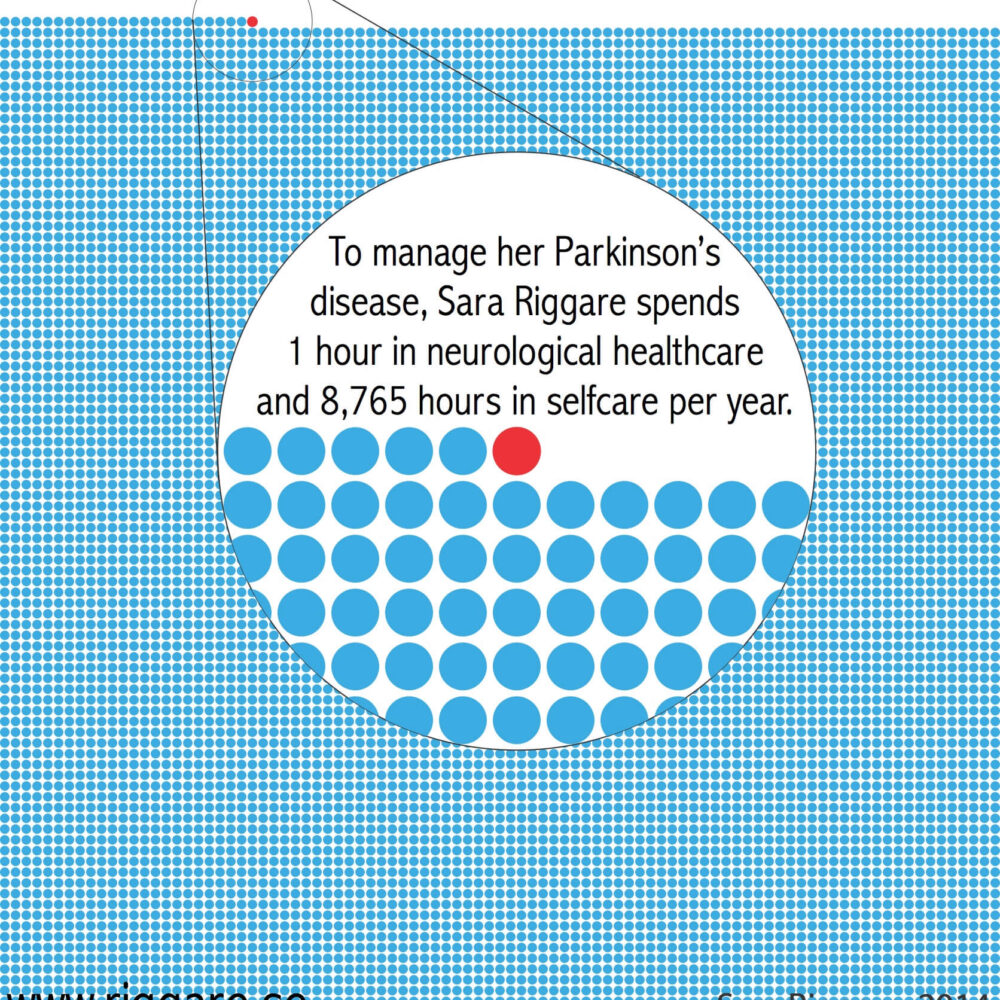
In 2014, she created an infographic to represent the hours she spends taking care of herself each year (8,765) versus the time she spends with a neurologist (30 minutes, twice a year, so 1 hour total).
As she wrote at the time:
I take 6 prescription drugs, 6 times a day, in 5 different combinations, with 6 different time intervals. Because let’s face it, my doctor doesn’t even know if I take my medications or not.
It is also during my 8,765 hours of selfcare that I can observe the effects of my treatment. And what if I could register my observations in a systematic way and bring to my next neurologists’ visit?
Guess what? I already am!
I am not saying I want more time in healthcare. I really don’t think I need more time with my neurologist. However, I am saying that healthcare needs to acknowledge the work we patients do in selfcare and also start working to make use of our observations for their own knowledge.
Just imagine what we could achieve if we start working together – as equals with different but complementary areas of expertise!
Her infographic quickly spread across the world as an arresting image of patient-led care and can now be downloaded in Swedish, English, Spanish, Italian, and German.
More recently, Riggare started creating necklaces to make the same point. Each one has 364 beads of one color and 1 bead of another color to represent the contrast between the time she spends caring for her health on her own versus the time spent with clinicians. She adds a dopamine molecule pendant to signify that neurotransmitter’s role in Parkinson’s disease. I proudly wear my necklace to health care conferences and use it as a conversation starter, much in the same way I wear my Walking Gallery jacket, painted by Regina Holliday.

(One of my favorite color combinations is pictured above with my dog providing the backdrop.)
What are some other examples of ways to draw attention to home truths like self care? Do you carry or wear symbols of your identity as a patient, survivor, or caregiver? Please share in the comments.
To learn more about Riggare’s research, check out her PhD thesis, “Personal Science in Parkinson’s Disease.“
Sara’s graphic is/was so powerful, in conveying the reality that we (patients/family) do almost all the work of caring for ourselves.
However, a slight historical correction to your post … Sara’s original diagram dates from 2012 (well … the first version I saw). I used it on the cover slide of my September 2013 keynote at Stanford’s MedX, which was titled “Health Technology for the other 99%”. Which was more or less the same keynote I’d presented in Stockholm (at Sara’s invitation) in May 2013.
I love the infographic! I was doing a talk somewhere about integrative oncology and did the math in my head. For my two cancers, my treatment is currently :30 once every 28 days. That’s about a .25 of a % so the other 99.75% of my month I am treating my cancers in more integrative ways. Everyone focuses on the .25 while they should be focusing on the 99.75!
Right?? One of my children lives with life-threatening food allergies. During the early years, when we had not yet identified all the triggers, we kept a go-bag by the front door because we had to rush to the ER six times before age 5 (salmon, sesame, chick peas, some tree nuts, and the list goes on). Every year we would train teachers and after-school aides how to recognize the signs of anaphylaxis and what to do (epinephrine immediately, then an antihistamine, then call 911).
At the end of every school year we would get the med pack back, hopefully intact since there had been no emergencies, and I wanted there to be some ceremony, some acknowledgment that we had all done an extraordinary job.
All that care, annually, including vigilance by the kid advocating for themselves, goes uncelebrated, unacknowledged: 1,460 potential triggers in one year (3 meals and a snack, every day, without incident x 365).
A home truth we’re learning more about is how disparate “self-care” is with the burden of having to coordinate care across multiple providers, labs, pharmacies while navigating different hospital systems & finding providers who know about cystic fibrosis or are willing to learn. Given the increasingly variable nature in which CF is experienced by those living with the condition, individualized care assumes baseline understanding of the disease from which to make shared decisions. There’s also much that we don’t know as people live longer with CF and with longevity, comes the luxury of accumulating comorbidities.
Trying to find specialists and primary care providers who are willing to take you on – so that you can do more self-care w/ trusted partners begs the question, how much do I reveal about myself and all I have to do in between visits? To Sara’s point, this “self-care” is where she spends all but 1 hour of her life in a calendar year. Graphic that conveys what patients do in between visits here:
https://drive.google.com/file/d/17ur5TiIKZUvFzH2ZVjUSdi4VZMzbShkS/view?usp=sharing
QT, my apologies for being slow to approve your great comment! The link didn’t work for me so please try again (or email me a screenshot and I’ll post it).
We are living in interesting times to say the least and I was focused on national political news instead of my own work.