While writing my upcoming book, Rebel Health, I dove into the history of innovation and of the patient-led scientific revolution. I read the daring adventures of caregivers, survivors, and patients who pushed the edges of what is possible in medicine. I learned about clinicians’ and researchers’ perspectives on the changes happening in health care. And […]
Tom Ferguson
Credible, useful, helpful, trustworthy
Inspired by a conversation with my FasterCures colleagues, I began looking into survey data related to trust and credibility, particularly: What entities and resources do people turn to when they need advice about important topics? Edelman, a global communications firm, has been measuring trust and credibility for 20 years. Their most recent Trust Barometer asked […]
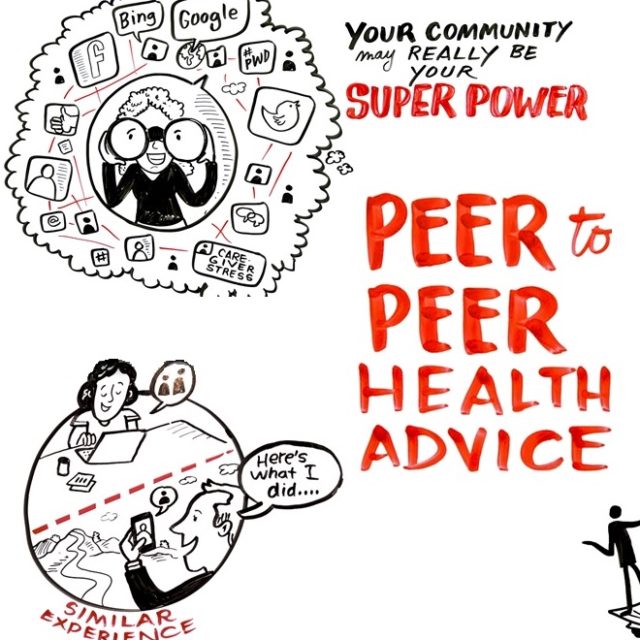
How peer-to-peer health advice can help people take their meds on time (and so much more)
(Yes, it’s the third post in 5 days from me, but when you’ve got cool stuff to share, why wait?) Matthew Zachary‘s podcast, Out of Patients, is one of my favorites because he brings his whole self to health care discussions, as you’ll hear in our conversation. It was a pleasure to unpack my latest […]
Well/Connected
Dr. Joe Kvedar interviewed me for his podcast, Well/Connected, and I thought I’d share footnotes for all the resources I mentioned. Key findings from the national survey of 14- to 22-year-olds focused on digital health and social media use, sponsored by Hopelab and Well Being Trust, which took a special look at people living with […]
What do you keep nearby, to inspire you?
Tom Ferguson, MD, gave me this robot in 2002, part of the first (and only?) fourth class of awardees of the Ferguson Report Distinguished Achievement Awards. I have kept it on or near my desk ever since. Reading Tom’s old essays, even as far back as the 1970s, is humbling. He foresaw so much of the world […]
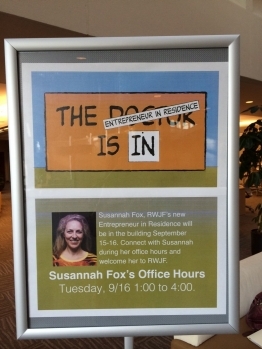
I’m RWJF’s Newest Entrepreneur in Residence
This post originally appeared on RWJF’s Culture of Health blog: I am thrilled to begin my job as the entrepreneur in residence (EIR) at the Robert Wood Johnson Foundation. You might think that the EIR role is traditionally associated with venture capital firms, not foundations. But scratch the surface and you’ll find commonalities between the two industries. […]



Recent Comments