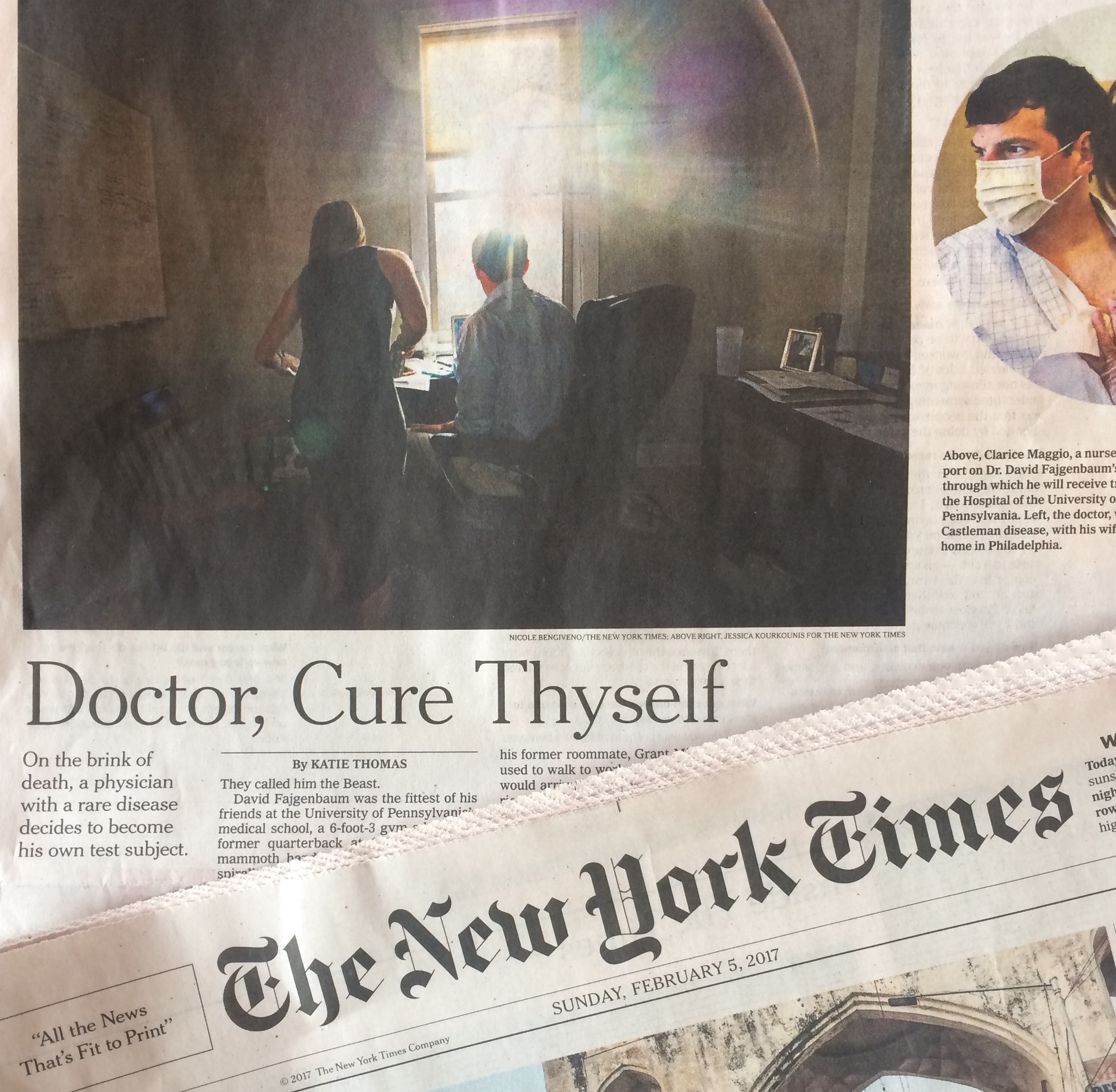
How might we empower people to participate in research about their own diseases or conditions? Which models work best for organizations solving medical mysteries or improving care for those living with rare conditions? These are two of the questions raised by a New York Times story today: “His doctors were stumped. Then he took over,” by Katie Thomas […]
C3N Project
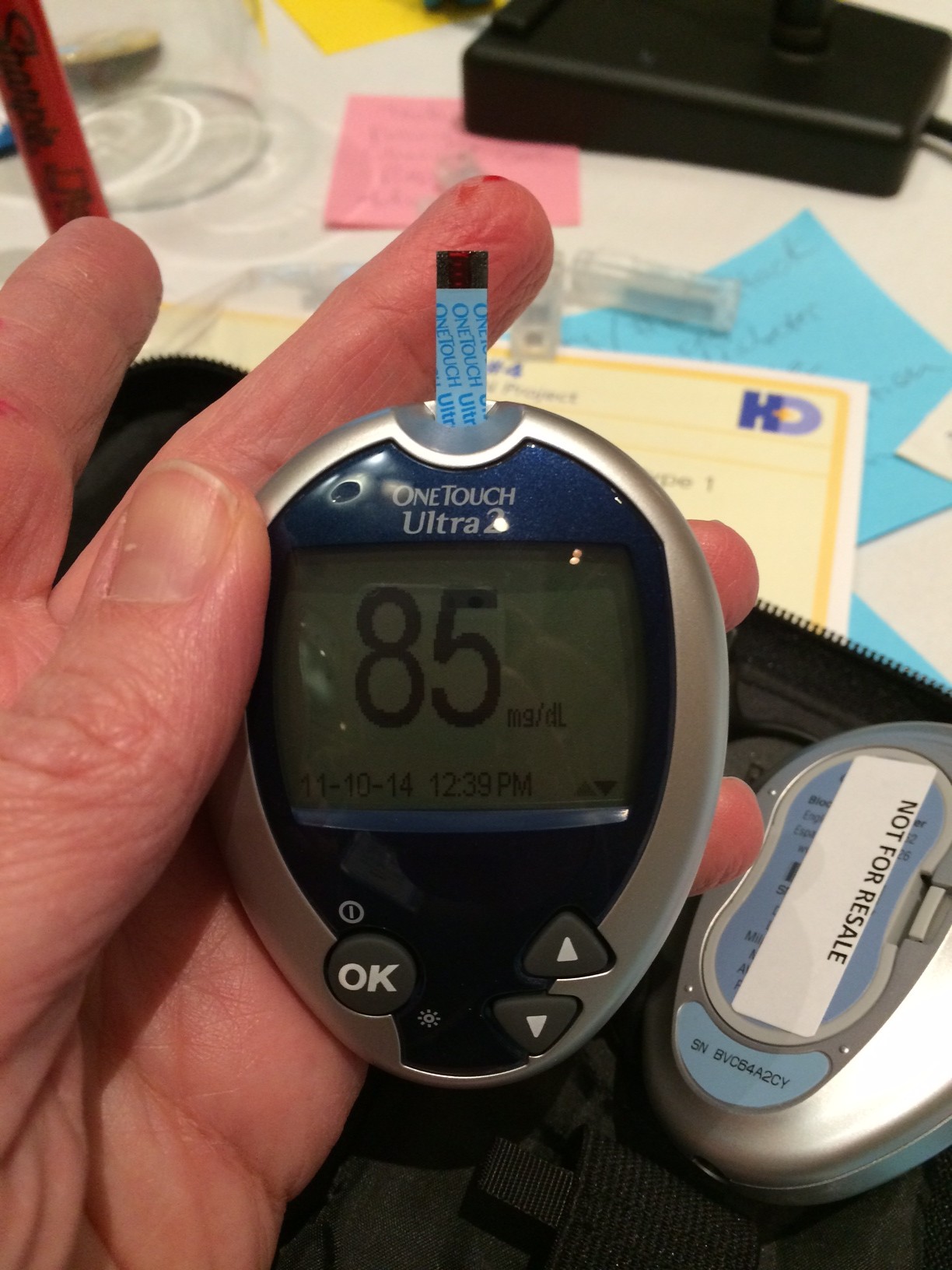
Imagining better outcomes for T1D with #MakeHealth
This post originally appeared on Diabetes Mine. Forty-five makers, thinkers, designers and doers gathered in Cincinnati for a two-day meeting to kick off “Phase Zero” of a new initiative to imagine a new system of care for people living with Type 1 diabetes (T1D). The best way I can describe the group is that everyone […]
How did we get here? And where are we going?
Video of my talk in Sweden is now online (skip to minute 7 unless you speak Swedish): It’s a comprehensive summary of my research so far, as well as an argument for listening to patients and caregivers as we move forward into the future. I opened with an example that was inspired by a visit […]
Peer-to-peer health care is a slow idea that will change the world
2018 update: Watch a 10-minute video that captures the essentials of peer health advice. Someone recently asked me to name the most exciting innovation in health care today. I think he was hoping for a sexy technology tip, like an app that’s catching fire in the expert patient communities I follow. Nope. I’ve said it […]
What’s your health care dream?
Note: This is two posts in one — scroll down to read Regina Holliday’s point of view. From Susannah Fox: For me, Twitter is a free-wheeling space where people dance with ideas. Anyone is welcome to jump into the spotlight and take a twirl. That’s how I see hashtags – spotlights on circles of people, […]


Recent Comments